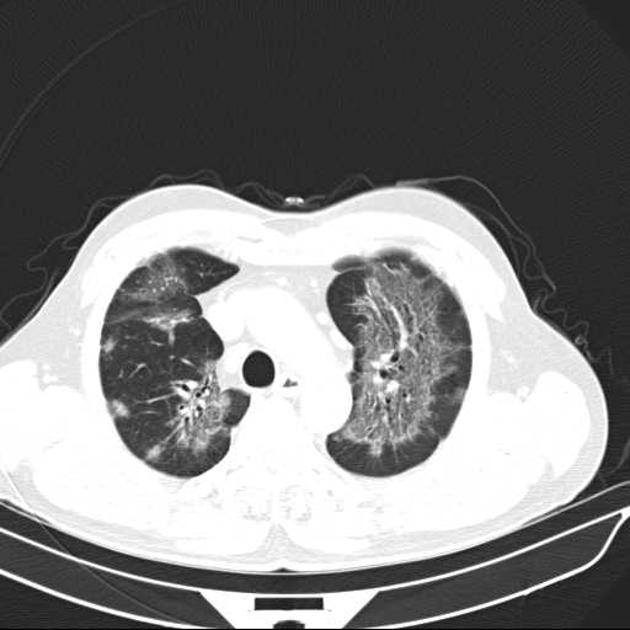
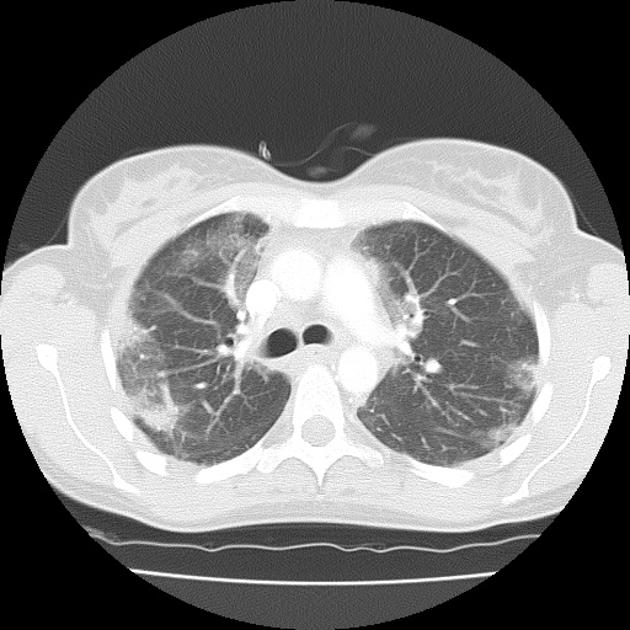
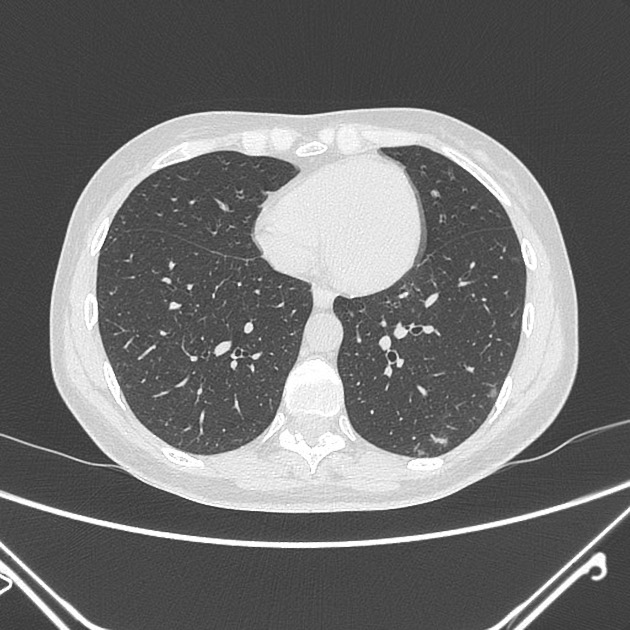
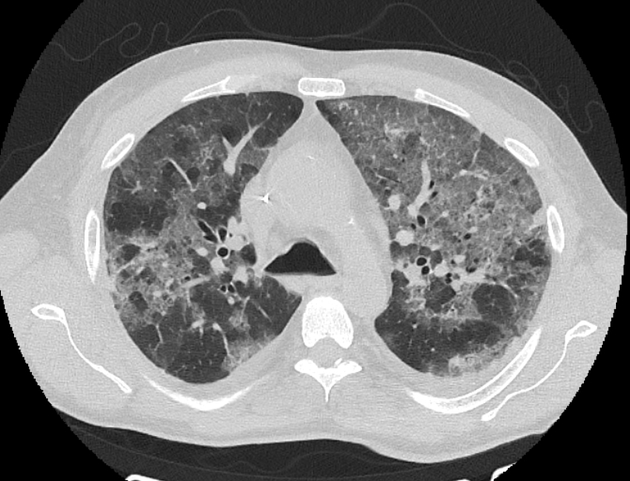
Ground-glass opacification/opacity (GGO) is a descriptive term referring to an area of increased attenuation in the lung on computed tomography (CT) with preserved bronchial and vascular markings. It is a non-specific sign with a wide aetiology including infection, chronic interstitial disease and acute alveolar disease.
Although the term was first used as a radiograph descriptor, and this use being in previous iterations of the Fleischner glossary 7, it is currently (c. 2024) recommended to reserve the term for CT only 9.
'Ground glass' derives from an industrial technique in glassmaking where the surface of normal glass is roughened by grinding it.
On this page:
Images:
Pathology
Aetiology
Ground-glass opacities have a broad aetiology, caused by any process that partially fills the alveolar space and is below the resolution of CT 9:
normal expiration
partial filling of air spaces with oedema, haemorrhage, or cellular fluid
partial collapse of alveoli
interstitial thickening
fibrosis
lepidic proliferation of neoplasm
Morphological forms
focal ground-glass opacification (includes ground-glass nodules)
diffuse ground-glass opacification (includes diffuse ground-glass nodules)
Differential diagnosis
Broadly speaking, the differential for ground-glass opacification can be split into 5:
infectious processes (opportunistic vs non-opportunistic)
chronic interstitial diseases
acute alveolar diseases
other causes
To narrow down the differential diagnosis, following points may be of help 8:
Is the GGO pathological?
if the membranous posterior wall of the trachea bows anteriorly, the scan has been performed in expiration and lung attenuation will be increased.
dependent atelectasis is a common normal finding. If the extent is greater than normal, prone imaging can differentiate normal from abnormal
if mosaic attenuation pattern is present, attenuation measurements help to distinguish normal from abnormal
What is the time course of the GGO?
acute GGO lasts only days or weeks. In this setting, imaging is less important as the most common causes of acute GGO (infection, oedema, haemorrhage, ARDS, and non-fibrotic hypersensitivity pneumonitis) may have overlapping and non-specific features. The clinical features are the key to diagnosis
chronic GGO may remain relatively unchanged for many weeks and even years. In these case the spatial distribution and additional imaging findings are important
recurring GGO (e.g., haemorrhages in vasculitis), is a potential pitfall when assessing the time course
recent bronchoalveolar lavage may alter the attenuation in both directions (i.e., increasing attenuation through remaining fluid, and decreasing attenuation after treating pulmonary alveolar proteinosis)
What is the spatial distribution?
upper zone predominant GGO may occur in hypersensitivity pneumonitis, respiratory bronchiolitis and sarcoidosis
mid and lower zone predominant GGO may occur in non-specific interstitial pneumonia, desquamative interstitial pneumonia, pulmonary oedema, and aspiration
GGO in the peripheral zone may occur in non-specific interstitial pneumonia, desquamative interstitial pneumonia, organising pneumonia and eosinophilic pneumonia
GGO in the central zone may occur in hypersensitivity pneumonitis, diffuse alveolar haemorrhage, pulmonary alveolar proteinosis, pulmonary oedema, and aspiration
Infections
Opportunistic
respiratory syncytial virus (RSV) bronchiolitis: type of infectious bronchiolitis
other infectious causes
Non-opportunistic
Chronic interstitial diseases
-
eosinophilic pneumonias: ground-glass opacification can be seen in many of the eosinophilic pneumonias but is most commonly seen in 2:
simple pulmonary eosinophilia (SPE): nodules with a GGO halo
idiopathic hypereosinophilic syndrome (IHS): nodules with a GGO halo
acute eosinophilic pneumonia (AEP): bilateral patchy areas of GGO with interlobular septal thickening
eosinophilic drug reactions: peripheral airspace consolidation and GGO
-
idiopathic interstitial pneumonias 3
non-specific interstitial pneumonia: GGO with linear or reticular markings, micronodules, consolidation, and microcystic honeycombing
usual interstitial pneumonia (UIP): focal GGO with macrocystic honeycombing, reticular opacities, traction bronchiectasis, and architectural distortion
cryptogenic organising pneumonia (COP): formerly bronchiolitis obliterans with organising pneumonia (BOOP); GGO with airspace consolidation and mild bronchial dilatation
exudative phase of acute interstitial pneumonia (AIP): diffuse lung consolidation with GGO
respiratory bronchiolitis-associated interstitial lung disease (RB-ILD): patchy GGO centrilobular nodules and bronchial wall thickening
desquamative interstitial pneumonia (DIP): GGO with linear or reticular opacities
lymphoid interstitial pneumonia (LIP): GGO often in association with perivascular cystic lesions, septal thickening, and centrilobular nodules
Acute alveolar disease
hypersensitivity pneumonitis: especially acute and subacute forms
Other causes
-
neoplastic processes with a lepidic proliferation pattern
localised adenocarcinoma
adenocarcinoma in situ or minimally invasive (formerly bronchoalveolar cell carcinoma)
Rare causes
focal interstitial fibrosis: a non-neoplastic entity with a nodular ground-glass opacity that does not change over a long period of time; can be mistaken for a neoplastic process
aspergillosis: a nodule with surrounding ground-glass opacity (CT halo sign) is rare except in severely immunocompromised patients
traumatic lung injury (pulmonary contusion)
poisoning e.g. acute/subacute phase of paraquat poisoning
pulmonary cryptococcus infection: solitary or multiple pulmonary nodules with or without peripheral GGO








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.