Gyral enhancement
Citation, DOI, disclosures and article data
Citation:
Deng F, Hacking C, Fortin F, et al. Gyral enhancement. Reference article, Radiopaedia.org (Accessed on 18 Mar 2025) https://doi.org/10.53347/rID-73596
rID:
73596
Article created:
Disclosures:
At the time the article was created Francis Deng had no recorded disclosures.
View Francis Deng's current disclosures
Last revised:
Disclosures:
At the time the article was last revised Craig Hacking had no recorded disclosures.
View Craig Hacking's current disclosures
Revisions:
9 times, by
5 contributors -
see full revision history and disclosures
Systems:
Sections:
Synonyms:
- Gyriform enhancement
- Grey matter enhancement
- Cortical enhancement
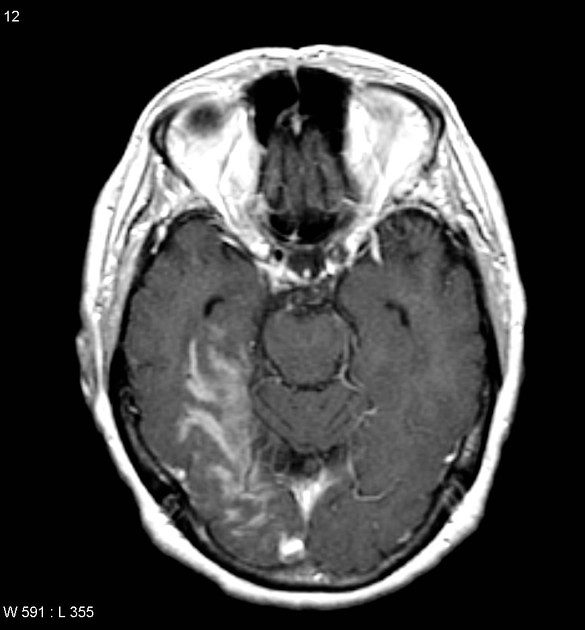
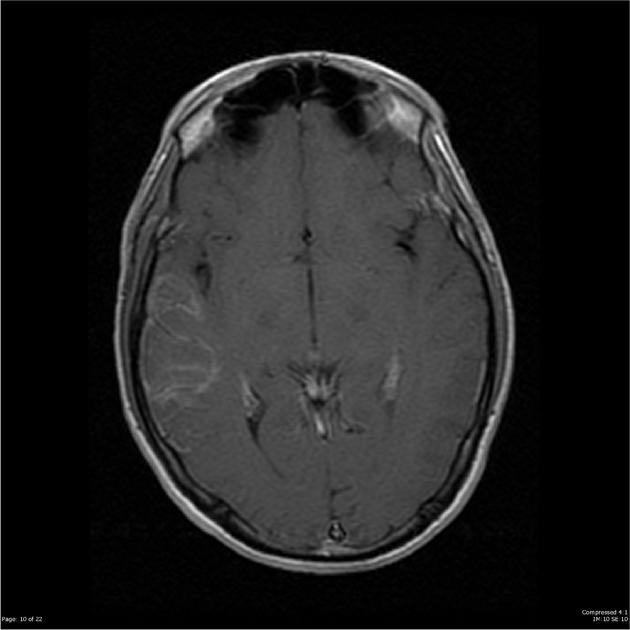
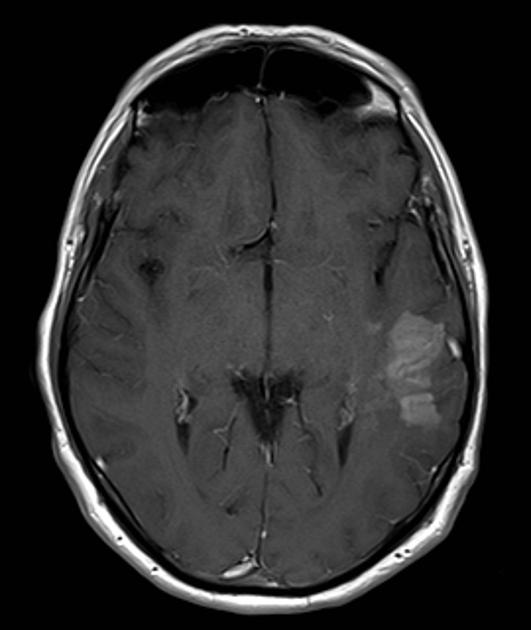
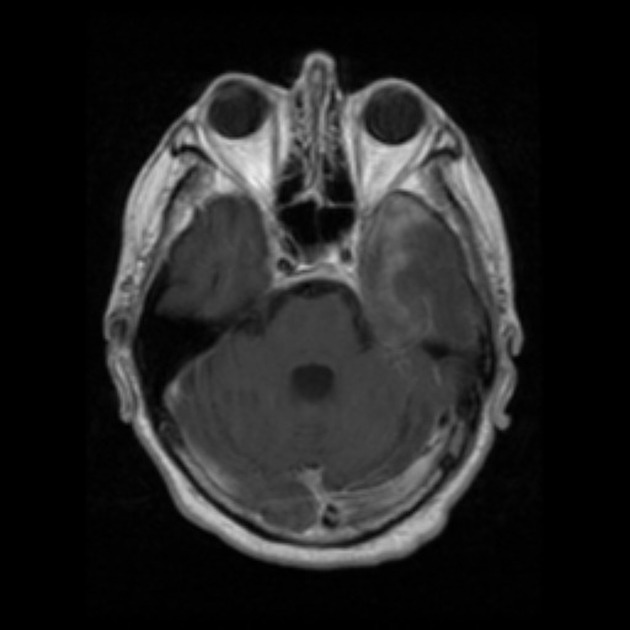
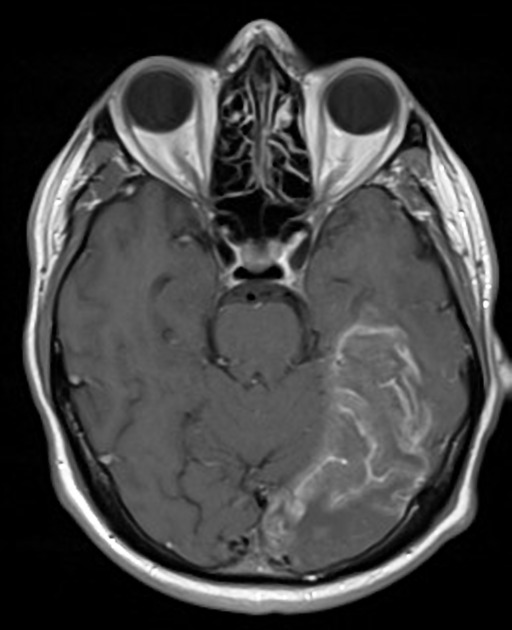
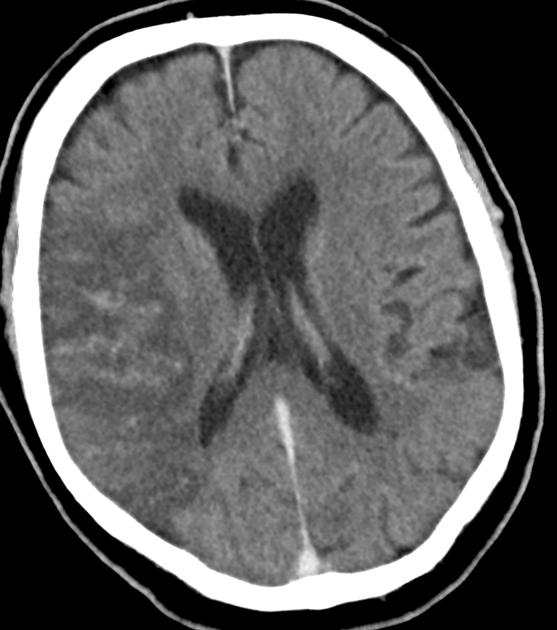
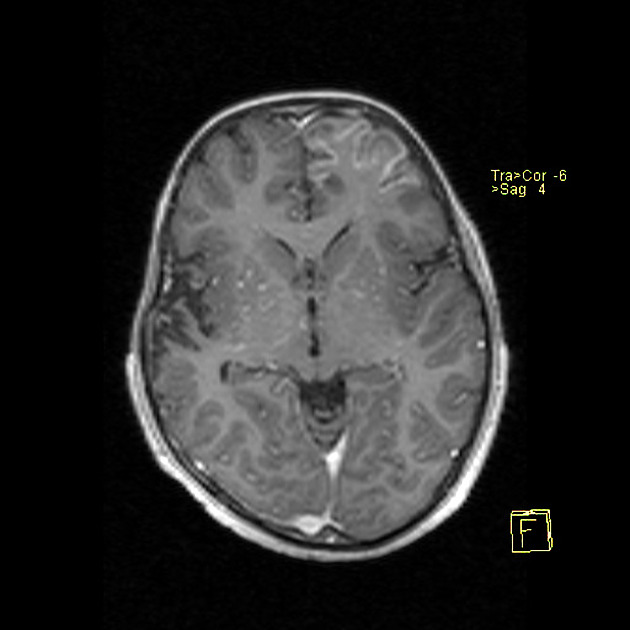
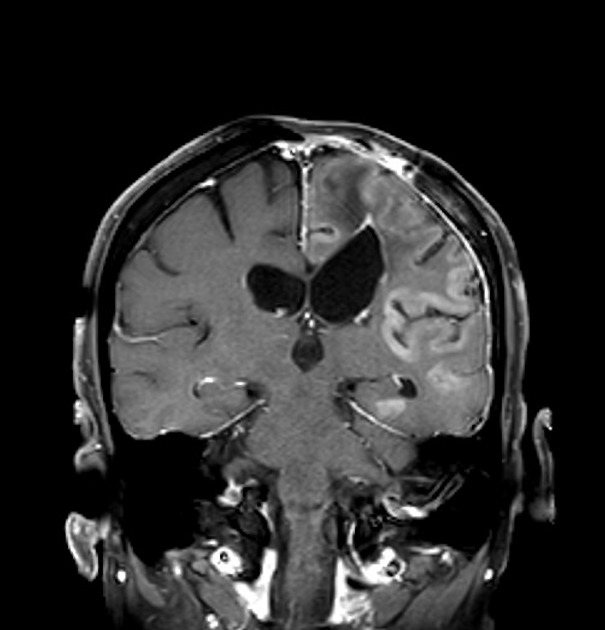
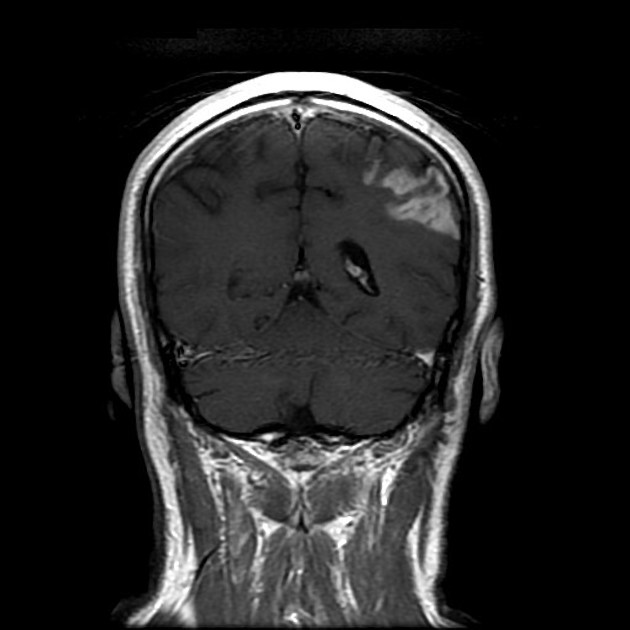
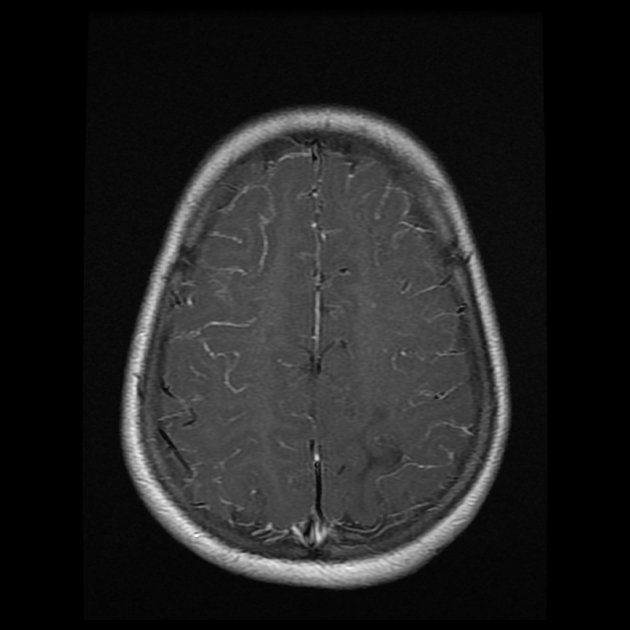
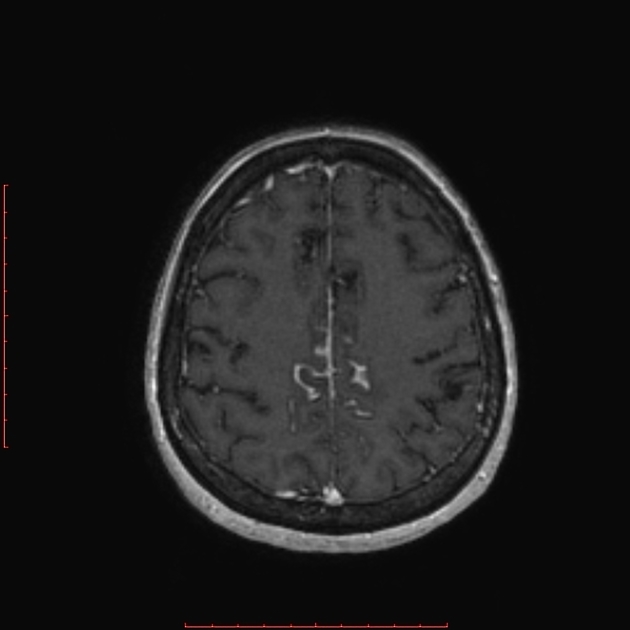
Gyral enhancement, also known as gyriform, cortical, or grey matter enhancement, is a pattern of contrast enhancement in the superficial brain parenchyma that conforms to the serpentine morphology of the cerebral gyri. It should be distinguished from leptomeningeal enhancement, which is also serpentine but occurs on the brain surface rather than within the parenchyma.
The causes are most commonly vascular or inflammatory, with subacute infarction being the most well described 1:
- vascular
- recent cerebral (cortical) infarction 2-7
- subacute infarct with luxury perfusion and/or cortical laminar necrosis (after 6 days until up to 4 months following stroke 26,27)
- acute ischaemic stroke after thrombolysis/thrombectomy
- venous infarct 8-10
- epileptic seizures (vasodilatory postictal state) 11,12
-
migraine
- migrainous infarction 15-18
- hemiplegic migraine 19,20
- stroke-like migraine attacks after radiation therapy (SMART) syndrome 21-23
- posterior reversible encephalopathy syndrome 24,25
- recent cerebral (cortical) infarction 2-7
- inflammatory/infectious
- neoplastic
- toxic
- cortical laminar necrosis related to drug toxicity (immunosuppressants and chemotherapy) 14
These causes may be distinguished by clinical history and brain location.
References
- 1. Smirniotopoulos JG, Murphy FM, Rushing EJ, Rees JH, Schroeder JW. Patterns of contrast enhancement in the brain and meninges. (2007) Radiographics : a review publication of the Radiological Society of North America, Inc. 27 (2): 525-51. doi:10.1148/rg.272065155 - Pubmed
- 2. Weisberg LA. Computerized tomographic enhancement patterns in cerebral infarction. (1980) Archives of neurology. 37 (1): 21-4. doi:10.1001/archneur.1980.00500500051006 - Pubmed
- 3. Imakita S, Nishimura T, Naito H, Yamada N, Yamamoto K, Takamiya M, Yamada Y, Sakashita Y, Minamikawa J, Kikuchi H. Magnetic resonance imaging of human cerebral infarction: enhancement with Gd-DTPA. (1987) Neuroradiology. 29 (5): 422-9. doi:10.1007/bf00341737 - Pubmed
- 4. Masdeu JC. Infarct versus neoplasm on CT: four helpful signs. (1983) AJNR. American journal of neuroradiology. 4 (3): 522-4. Pubmed
- 5. Cordes M, Henkes H, Roll D, Eichstädt H, Christe W, Langer M, Felix R. Subacute and chronic cerebral infarctions: SPECT and gadolinium-DTPA enhanced MR imaging. (1989) Journal of computer assisted tomography. 13 (4): 567-71. doi:10.1097/00004728-198907000-00003 - Pubmed
- 6. Castillo M, Scatliff JH, Kwock L, Green JJ, Suzuki K, Chancellor K, Smith JK. Postmortem MR imaging of lobar cerebral infarction with pathologic and in vivo correlation. (1996) Radiographics : a review publication of the Radiological Society of North America, Inc. 16 (2): 241-50. doi:10.1148/radiographics.16.2.8966284 - Pubmed
- 7. Hornig CR, Busse O, Buettner T, Dorndorf W, Agnoli A, Akengin Z. CT contrast enhancement on brain scans and blood-CSF barrier disturbances in cerebral ischemic infarction. (1985) Stroke. 16 (2): 268-73. doi:10.1161/01.str.16.2.268 - Pubmed
- 8. Buonanno FS, Moody DM, Ball MR, Laster DW. Computed cranial tomographic findings in cerebral sinovenous occlusion. (1978) Journal of computer assisted tomography. 2 (3): 281-90. doi:10.1097/00004728-197807000-00008 - Pubmed
- 9. Rao KC, Knipp HC, Wagner EJ. Computed tomographic findings in cerebral sinus and venous thrombosis. (1981) Radiology. 140 (2): 391-8. doi:10.1148/radiology.140.2.7255715 - Pubmed
- 10. Renowden S. Cerebral venous sinus thrombosis. (2004) European radiology. 14 (2): 215-26. doi:10.1007/s00330-003-2021-6 - Pubmed
- 11. Silverstein AM, Alexander JA. Acute postictal cerebral imaging. (1998) AJNR. American journal of neuroradiology. 19 (8): 1485-8. Pubmed
- 12. Dillon W, Brant-Zawadzki M, Sherry RG. Transient computed tomographic abnormalities after focal seizures. (1984) AJNR. American journal of neuroradiology. 5 (1): 107-9. Pubmed
- 13. Jinkins JR. Focal tuberculous cerebritis. (1988) AJNR. American journal of neuroradiology. 9 (1): 121-4. Pubmed
- 14. Bargalló N, Burrel M, Berenguer J, Cofan F, Buñesch L, Mercader JM. Cortical laminar necrosis caused by immunosuppressive therapy and chemotherapy. (2000) AJNR. American journal of neuroradiology. 21 (3): 479-84. Pubmed
- 15. Liang Y, Scott TF. Migrainous infarction with appearance of laminar necrosis on MRI. (2007) Clinical neurology and neurosurgery. 109 (7): 592-6. doi:10.1016/j.clineuro.2007.04.005 - Pubmed
- 16. Khardenavis V, Karthik DK, Kulkarni S, Deshpande A. Cortical laminar necrosis in a case of migrainous cerebral infarction. (2018) BMJ case reports. doi:10.1136/bcr-2017-221483 - Pubmed
- 17. Sharma SR, Massaraf H, Das S, Kalita A. Cortical Laminar Necrosis as a Presenting Manifestation of Migraine in an Apparently Normal Patient: A Rare Case Report. (2019) Journal of neurosciences in rural practice. 10 (3): 559-562. doi:10.1055/s-0039-1698009 - Pubmed
- 18. Arboix A, González-Peris S, Grivé E, Sánchez MJ, Comes E. Cortical laminar necrosis related to migrainous cerebral infarction. (2013) World journal of clinical cases. 1 (8): 256-9. doi:10.12998/wjcc.v1.i8.256 - Pubmed
- 19. Tee TY, Khoo CS, Raymond AA, Syazarina SO. Teaching NeuroImages: Neuroimaging in hemiplegic migraine. (2019) Neurology. 93 (6): e626-e627. doi:10.1212/WNL.0000000000007905 - Pubmed
- 20. Cha YH, Millett D, Kane M, Jen J, Baloh R. Adult-onset hemiplegic migraine with cortical enhancement and oedema. (2007) Cephalalgia : an international journal of headache. 27 (10): 1166-70. doi:10.1111/j.1468-2982.2007.01369.x - Pubmed
- 21. Black DF, Bartleson JD, Bell ML, Lachance DH. SMART: stroke-like migraine attacks after radiation therapy. (2006) Cephalalgia : an international journal of headache. 26 (9): 1137-42. doi:10.1111/j.1468-2982.2006.01184.x - Pubmed
- 22. Kerklaan JP, Lycklama á Nijeholt GJ, Wiggenraad RG, Berghuis B, Postma TJ, Taphoorn MJ. SMART syndrome: a late reversible complication after radiation therapy for brain tumours. (2011) Journal of neurology. 258 (6): 1098-104. doi:10.1007/s00415-010-5892-x - Pubmed
- 23. Maloney PR, Rabinstein AA, Daniels DJ, Link MJ. Surgically induced SMART syndrome: case report and review of the literature. (2014) World neurosurgery. 82 (1-2): 240.e7-12. doi:10.1016/j.wneu.2013.01.028 - Pubmed
- 24. McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, Teksam M. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. (2007) AJR. American journal of roentgenology. 189 (4): 904-12. doi:10.2214/AJR.07.2024 - Pubmed
- 25. Lamy C, Oppenheim C, Méder JF, Mas JL. Neuroimaging in Posterior Reversible Encephalopathy Syndrome. (2004) Journal of Neuroimaging. 14 (2): 89. doi:10.1111/j.1552-6569.2004.tb00223.x
- 26. Crain MR, Yuh WT, Greene GM, Loes DJ, Ryals TJ, Sato Y, Hart MN. Cerebral ischemia: evaluation with contrast-enhanced MR imaging. (1991) AJNR. American journal of neuroradiology. 12 (4): 631-9. Pubmed
- 27. Allen LM, Hasso AN, Handwerker J, Farid H. Sequence-specific MR imaging findings that are useful in dating ischemic stroke. (2012) Radiographics : a review publication of the Radiological Society of North America, Inc. 32 (5): 1285-97; discussion 1297-9. doi:10.1148/rg.325115760 - Pubmed





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.