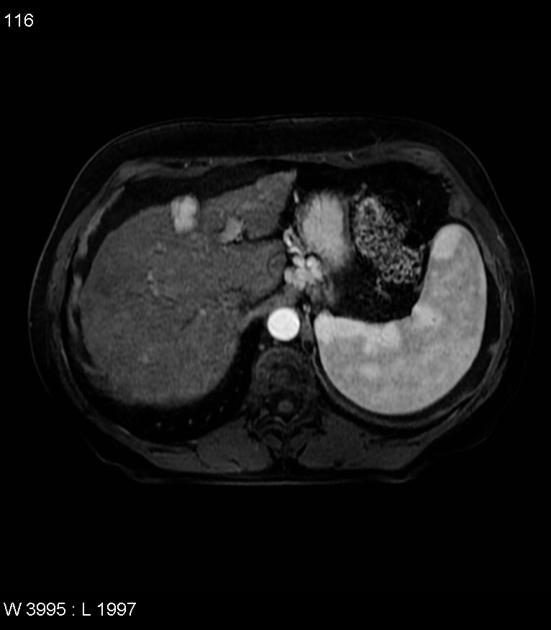
Hypervascular liver lesions are findings that enhance more or similarly to the background hepatic parenchyma in the late arterial phase on contrast-enhanced CT or MRI.
Differential diagnosis
Non-neoplastic
-
focal nodular hyperplasia (FNH)
bright arterial phase enhancement except central scar
isodense/isointense to liver on portal venous phase
central scar enhancement on delayed phase
-
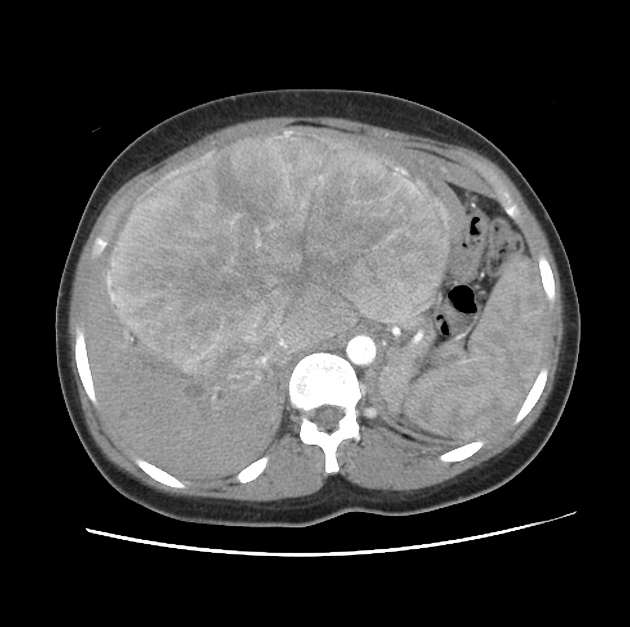
benign; most common liver tumour overall
discontinuous, nodular, peripheral enhancement starting in the late arterial phase
gradual central filling in
enhancement must match blood pool in each phase, or not a haemangioma (i.e. similar to the aorta in arterial, portal vein in portal phase, etc)
small haemangiomas (<1.5 cm) may demonstrate "flash filling" - complete homogeneous enhancement in arterial phase (no gradual filling in)
-
vascular shunts / fistulas
intrahepatic arterioportal shunt - arterioportal fistula 8
intrahepatic arteriovenous shunt - arteriovenous fistula
failing Fontan circulation 3
Neoplastic
-
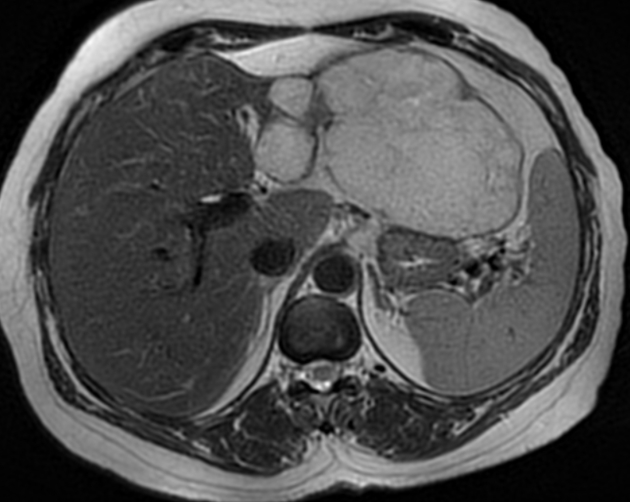
hepatocellular carcinoma (HCC)
most common hypervascular primary liver malignancy
early arterial phase enhancement and then rapid wash out
rim enhancement of capsule may persist
-
arterial phase: transient homogeneous enhancement
returns to near isodensity on portal venous and delayed phase image
Metastases
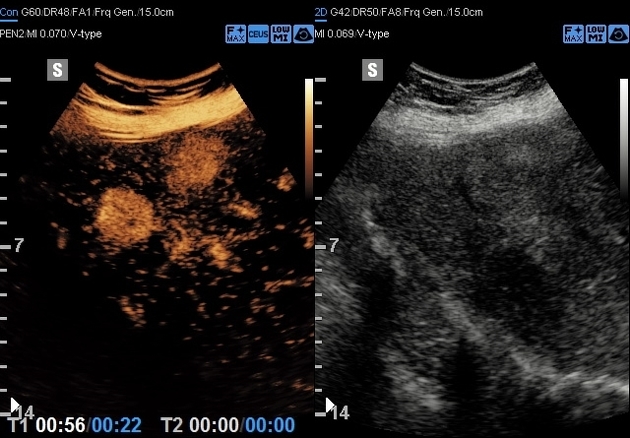
Although the majority of liver metastases are hypodense and enhance less than the surrounding liver, metastases from certain primaries demonstrate an increase in the number of vessels, resulting in a hyperechoic ultrasound appearance, and arterial phase hyperenhancement on CT or MRI which washes out on delayed scan (cf. haemangioma which does not show washout). The primaries typically include:








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.