Intracerebral hemorrhage (ICH), also known as intraparenchymal cerebral hemorrhage and often synonymously describing hemorrhagic stroke, is a subset of an intracranial hemorrhage as well as of stroke, defined by the acute accumulation of blood within the brain parenchyma.
This article concerns non-traumatic intracerebral hemorrhages; traumatic hemorrhagic cerebral contusions are discussed separately.
On this page:
Terminology
By convention, intracerebral hemorrhage refers to macroscopically visible, recent hemorrhages. In contrast, cerebral microhemorrhages are discussed separately.
Clinical presentation
An intracerebral hemorrhage presents similarly to an ischemic stroke and there are no reliable clinical differentiators between the two. There is typically a rapid onset of focal neurological deficit, which varies depending on the specific area of the brain that is involved. Compared to ischemic stroke, there is more likely to be a decreased conscious state 11. Other common clinical features include 13:
headache
nausea and vomiting
seizure
Pathology
Intracerebral hemorrhages arise from rupture of a small blood vessel within the brain parenchyma or, less commonly, of a blood vessel adjacent to the parenchyma (e.g. jet hematoma).
Etiology
Non-traumatic intracerebral hemorrhages were historically etiologically divided according to whether or not they have an underlying structural lesion or bleeding diathesis.
-
spontaneous intracerebral hemorrhage presumed due to small vessel disease (formerly primary intracerebral hemorrhage 10)
-
secondary intracerebral hemorrhage: hemorrhage complicating some underlying structural lesion or bleeding diathesis
vascular malformation (e.g., brain arteriovenous malformation, cerebral cavernous malformation)
tumor (e.g., metastases, glioblastoma)
bleeding diathesis (e.g., anticoagulation therapy)
Etiologies more commonly seen in the pediatric or young adult demographic are discussed separately: see stroke in children and young adults.
Location
Non-traumatic intracerebral hemorrhages are classified by location, which vary by etiologic association 9.
lobar intracerebral hemorrhage: in any lobe(s) of the cerebral hemispheres in a cortical and/or subcortical location (excluding deep hemispheric and infratentorial regions)
-
non-lobar intracerebral hemorrhage: in deep hemispheric or infratentorial location
deep hemispheric (basal ganglia, thalamus, internal capsule)
Radiographic features
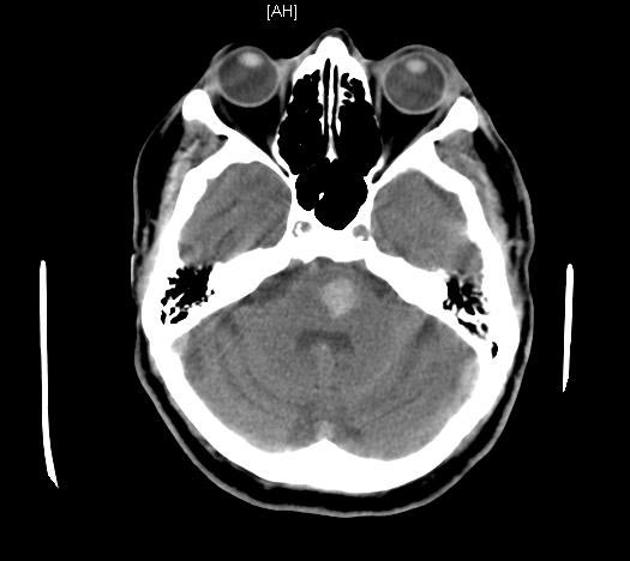
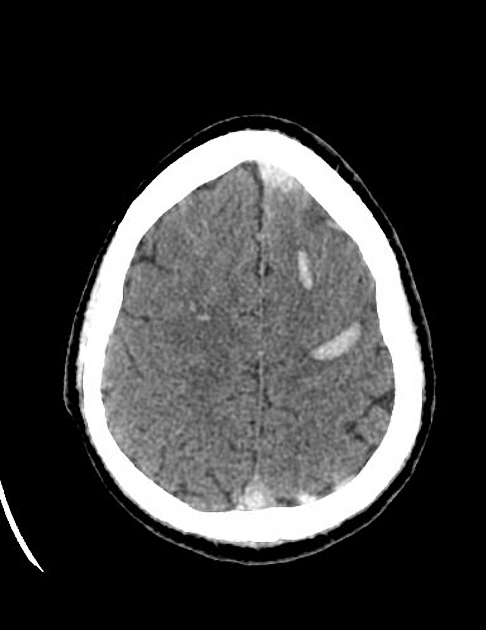
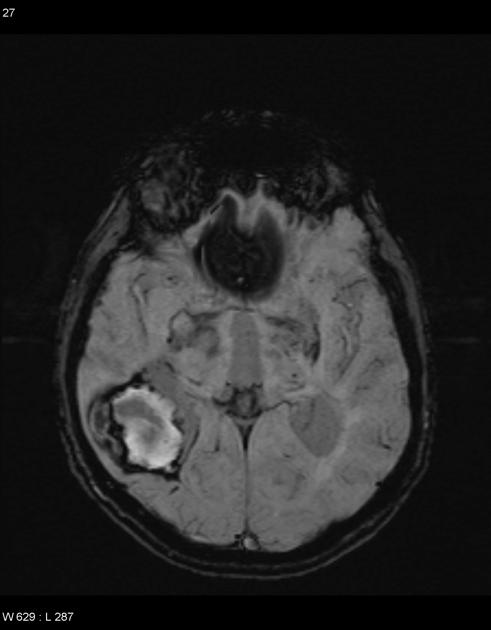
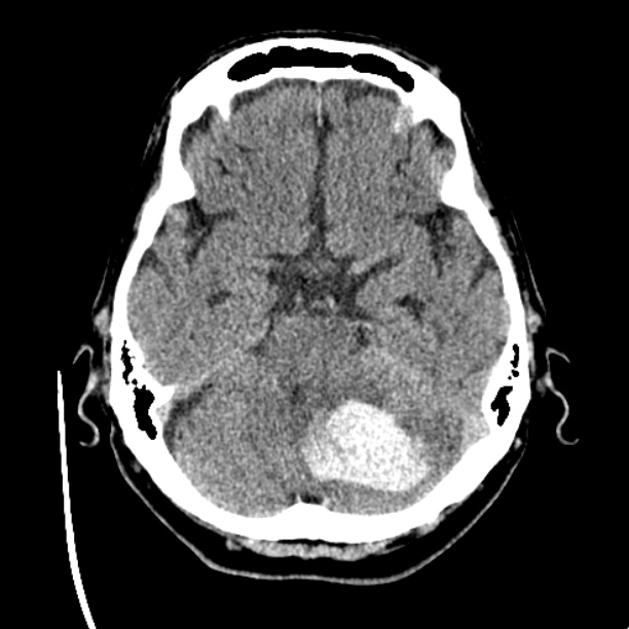
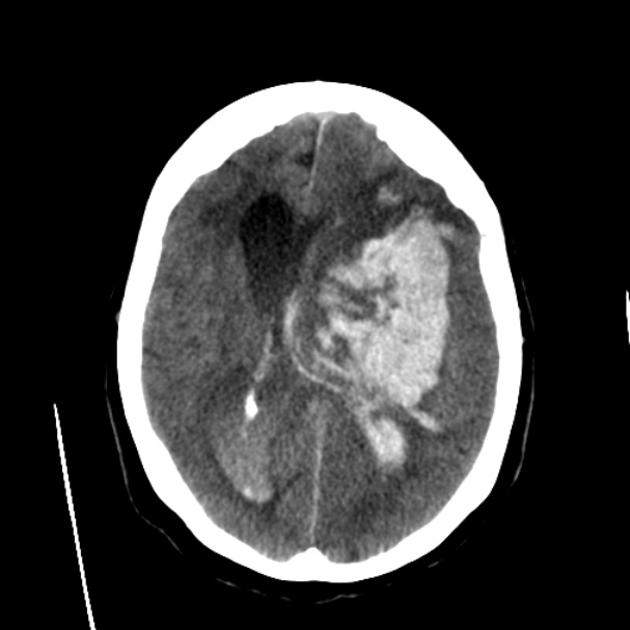
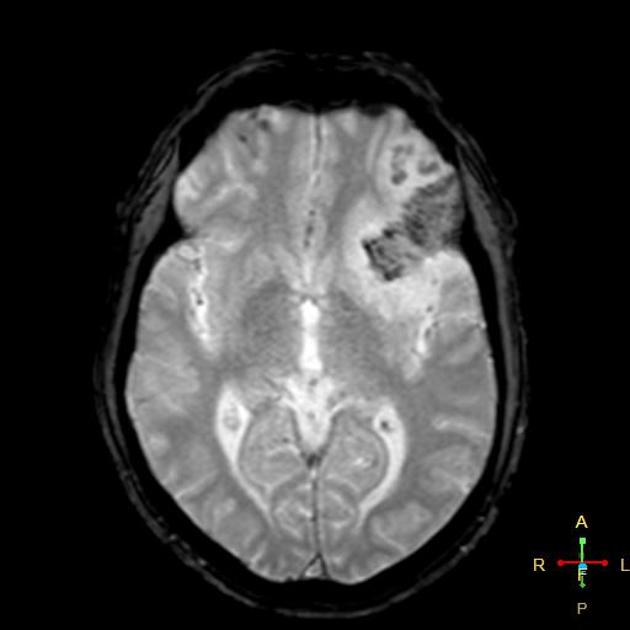
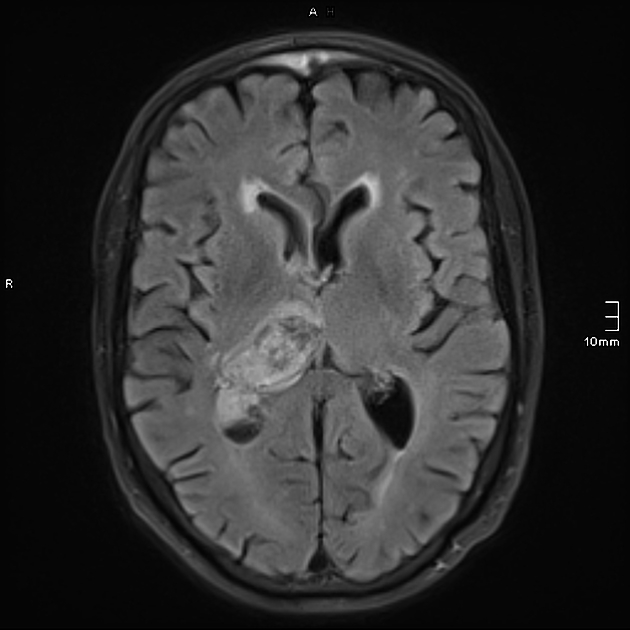
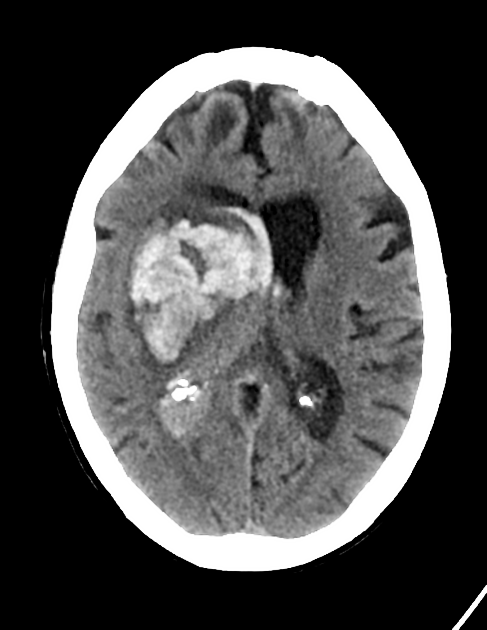
CT
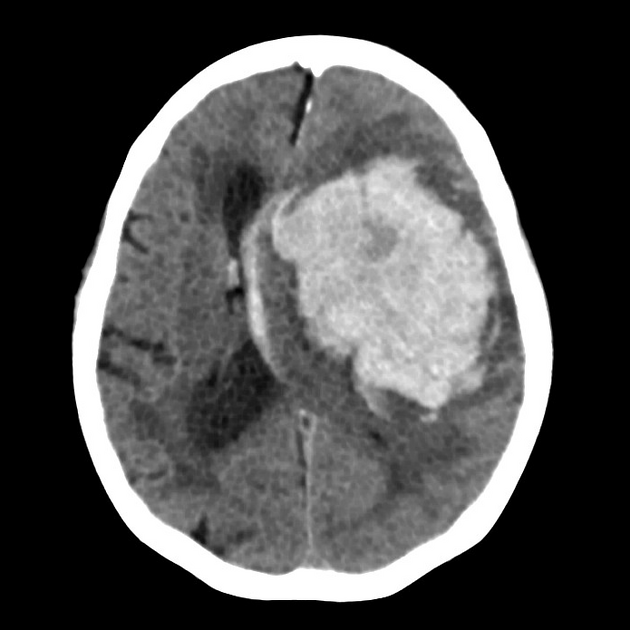
CT is usually the modality first obtained and demonstrates a hyperdense collection of blood, often with surrounding hypodense edema. A number of complications may be present, such as extension of the hemorrhage into other intracranial compartments, hydrocephalus, herniation, etc.
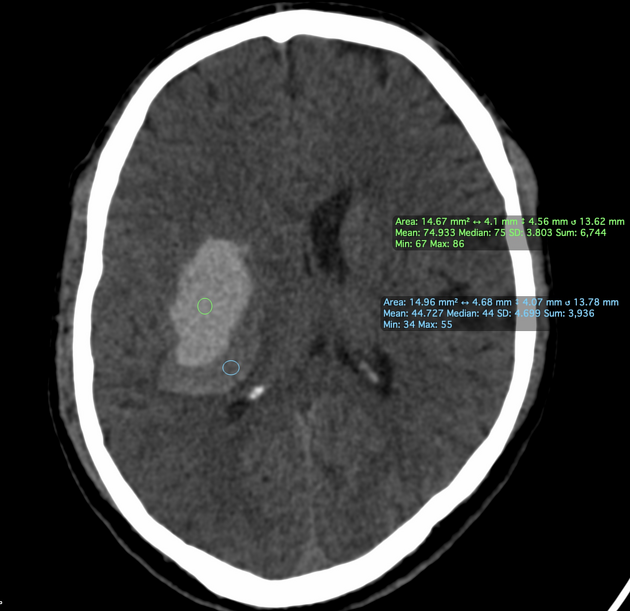
A number of CT features can predict the likelihood of hemorrhage expansion and are therefore useful in decision-making and prognosis.
-
non-contrast CT
-
hemorrhage size
the volume of an intracerebral hemorrhage can be measured using ABC/2 formula or 3D volumetric software
hemorrhage size is considered to be the most reliable independent predictor of ICH expansion
hematoma expansion is measured as an increased growth >12.5 mL or volume >33% from the initial CT scan
hematomas with a volume of more than 30 mL are more prone to expansion
-
hemorrhage shape
intracerebral hemorrhage irregularity is thought to be due to multiple leaking vessels feeding the hematoma
hemorrhages with irregular shapes are more prone to expansion
-
hemorrhage density
the presence of hypodense or isodense regions within the hyperdense intracerebral hemorrhage represents active bleeding and is called swirl sign
when the swirl sign is encapsulated it is termed black hole sign
the presence of a relatively hypodense area adjacent to a hyperdense area is termed the blend sign
heterogeneous hemorrhage with hypodense foci is more prone to expansion
-
intraventricular hemorrhagic extension
intraventricular hemorrhagic extension occurs due to decompression of the hemorrhage into the low resistance ventricular system, thus; hematomas located in the thalamus, caudate nucleus or pons are more prone to intraventricular extension than lobar hematomas
a study has shown that lenticular and lobar hematomas with accompanying intraventricular extension displayed a higher proportion of hematoma expansion 5
-
-
contrast-enhanced CT
active contrast extravasation within hematoma predicts future hemorrhage expansion, this can be observed on CT angiography (CTA) as spot sign and pooling of contrast within the hematoma
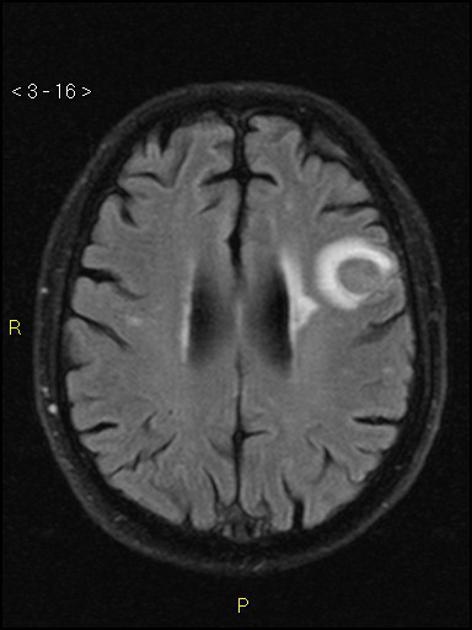
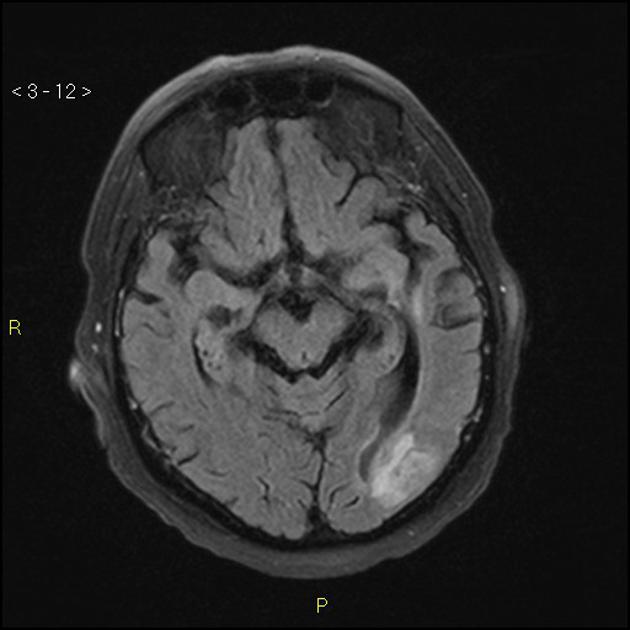
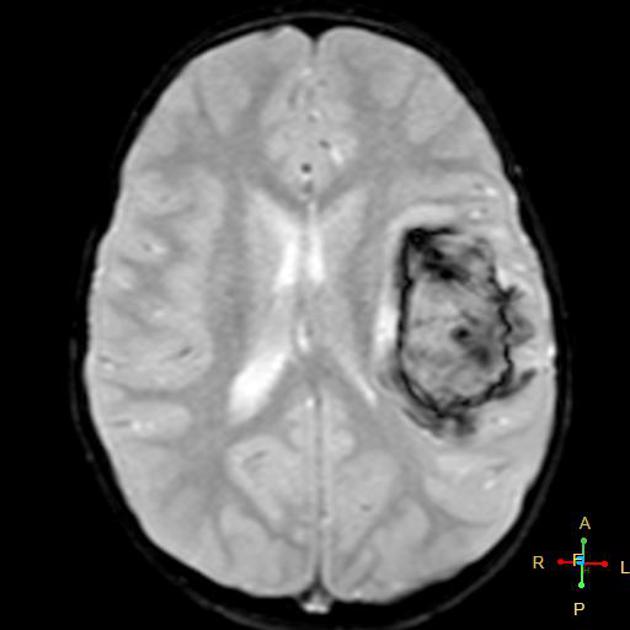
MRI
Findings depend on the size and age of the bleed (see aging blood on MRI). MRI may also reveal clues to the etiology, such as those of cerebral small vessel diseases (e.g. hypertensive microangiopathy, cerebral amyloid angiopathy).
Treatment and prognosis
Management is time-critical 14,15, with the principles of management including 12:
control of blood pressure, aiming for a systolic blood pressure of ~140 mmHg
-
reversal of any anticoagulation or coagulopathy
there is a paucity of evidence to support the effectiveness of routine use of hemostatic agents
-
management of raised intracranial pressure
e.g. external ventricular drain in the acute setting (especially if there is concurrent intraventricular hemorrhage), decompressive hemicraniectomy (weak evidence to support this in deep intracerebral hemorrhage 17)
-
neurosurgical hematoma evacuation can be considered on a case-by-case basis
evidence to support hematoma evacuation with or without extraventricular drain in cerebellar intracerebral hemorrhage 12, minimally invasive evacuation techniques in lobar intracerebral hemorrhage 16
-
management of seizures with antiseizure medications
there is a paucity of evidence to support the effectiveness of antiseizure medication prophylaxis for patients without seizures
Additionally, supportive care should be provided, including caring for patients in dedicated inpatient stroke units and attempting to prevent the numerous complications which are encountered by patients with neurological impairment from stroke.
Practical points
With any intracerebral hemorrhage the following points should be included in a report as they have prognostic implications 3:
location
-
size/volume
the ABC/2 formula is widely used, but there may be more accurate formulas (e.g. 2.5ABC/6, SH/2) and analyzes available, some of which, however, may require the addition of specific software to the standard PACS tools
shape (irregular vs regular)
density (homogeneous vs heterogeneous)
presence/absence of substantial surrounding edema that may indicate an underlying tumor
presence/absence of intraventricular hemorrhage
presence/absence of hydrocephalus
when CT angiography is performed, the presence/absence of the CTA spot sign or a vascular malformation








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.