Leptomeningitis, which is more commonly referred to as meningitis, represents inflammation of the subarachnoid space (i.e. arachnoid mater and pia mater) caused by an infectious or non-infectious process.
On this page:
Pathology
Aetiology
Infective
-
-
elderly
Streptococcus pneumoniae
Listeria monocytogenes
Neisseria meningitidis
Gram negative bacilli
-
adults
Streptococcus pneumoniae
Neisseria meningitidis
Group B streptococcus
-
children
Neisseria meningitidis
-
infants
Streptococcus pneumoniae
Neisseria meningitidis
-
neonates
Group B streptococcus
Escherichia coli
Listeria monocytogenes
-
-
Enterovirus
Herpesviruses
-
mycobacterial meningitis
-
Mycobacterium tuberculosis
-
-
fungal meningitis
Cryptococcus neoformans (in patients with AIDS)
Coccidioides immitis
-
protistic meningitis (often causing eosinophilic meningitis) 7
Angiostrongylus cantonensis
Gnathostoma spinigerum
For a further discussion related to other aetiological agents and other infective processes in the CNS, please refer to CNS infectious diseases.
Aseptic meningitis
-
iatrogenic
postoperative 4
hydrogel-coated aneurysm coils 3
NSAID-induced 8
Radiographic features
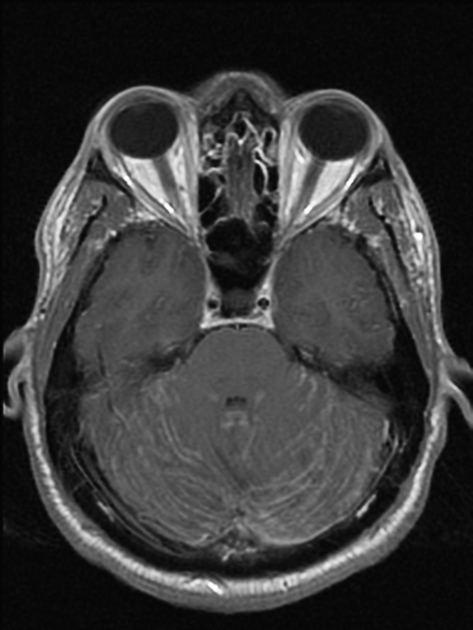
CT
may be normal
subtle hydrocephalus
hyperdensity around basal cisterns (especially in tuberculosis)
complications or sources of the meningitis
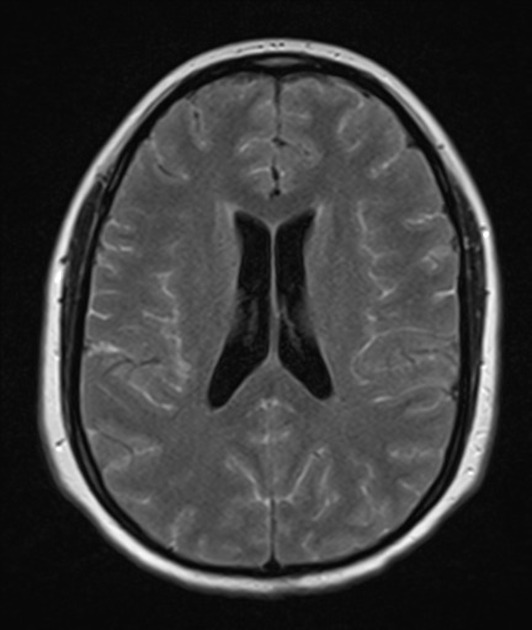
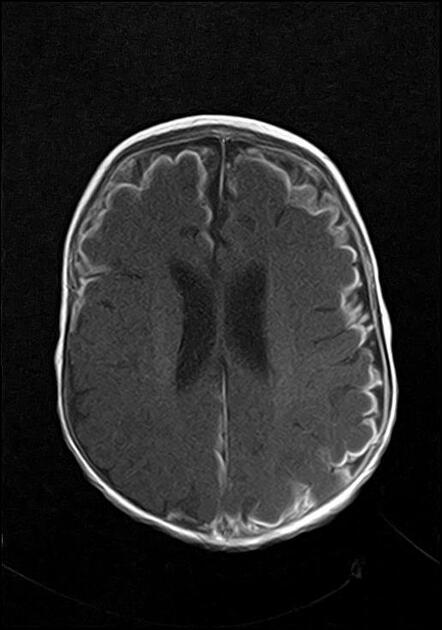
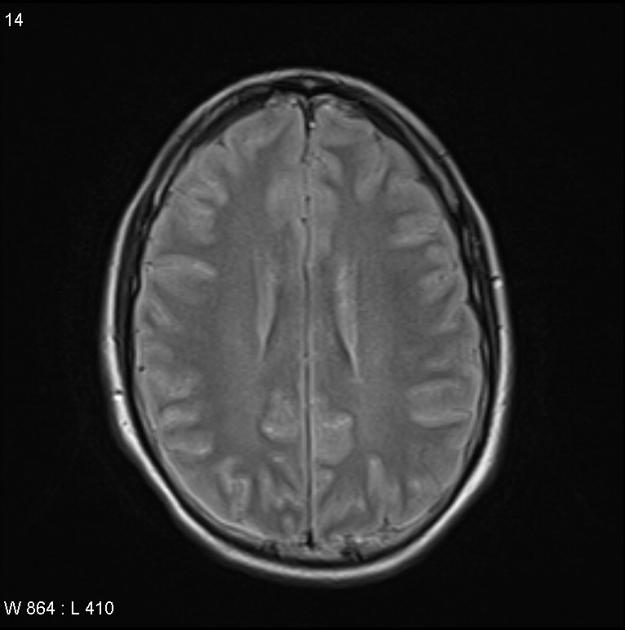
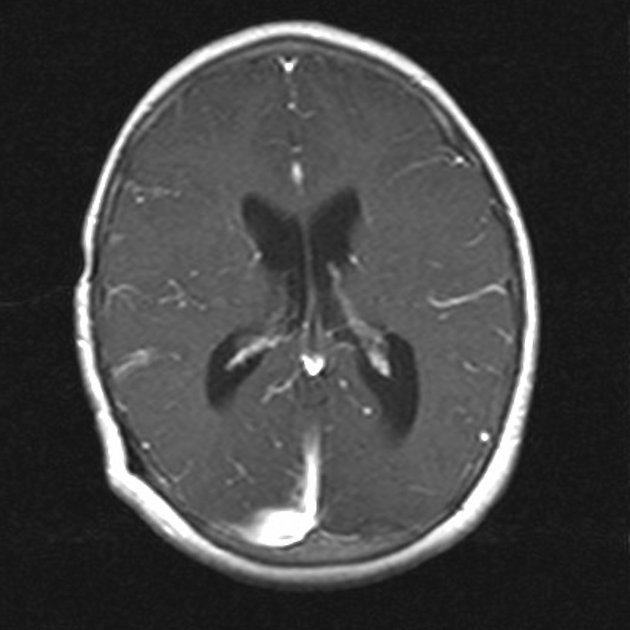
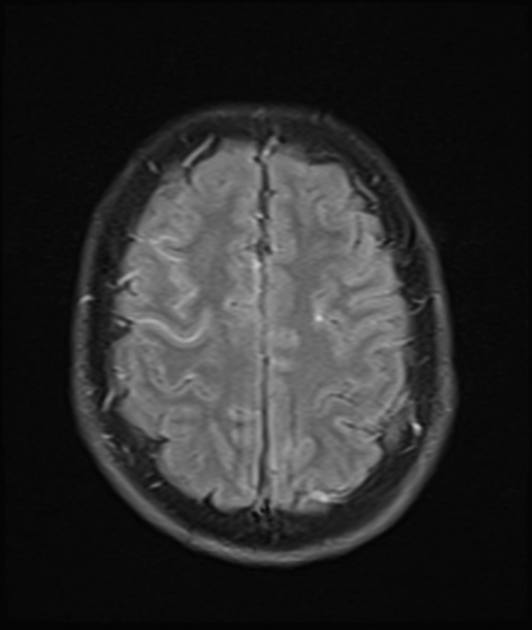
MRI
T1: may be normal; sulci may appear less hypointense than normal
T1 C+ (Gd): leptomeningeal enhancement
FLAIR: demonstrates hyperintense signal in CSF space, especially in the sulci
FLAIR C+ (Gd): has shown to be more sensitive and specific than T1 C+ (Gd) sequence in spotting leptomeningeal enhancement 6
MR angiography: arterial narrowing or occlusion
Treatment and prognosis
Complications
The complications of meningitis can be remembered using the mnemonic HACTIVE.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.