Myocarditis (rare plural: myocarditides) is a general term describing the inflammation of the heart muscle or myocardium and usually refers to non-ischemic myocardial inflammation and the different forms of myocarditis 1,2.
However myocardial inflammation can be also seen in the setting of myocardial ischemia and infarction, after myocardial reperfusion or in the setting of cardiac transplant rejection 4.
On this page:
Terminology
The following terms have been used in the context of non-ischemic myocardial inflammation and myocarditis by an expert panel 1:
acute myocarditis: non-ischemic myocardial inflammation with symptoms of recent onset, usually ≤1 month, increased levels of high-sensitive troponins and evidence of myocardial edema on cardiac MRI or positive cardiac FDG-PET
-
complicated acute myocarditis (working diagnosis): acute myocarditis with one or more of the following features:
cardiac dysfunction (LVEF <50%)
sustained ventricular arrhythmias
advanced heart block
low cardiac output syndrome
cardiogenic shock
-
fulminant myocarditis (working diagnosis): acute myocardial inflammation with rapid progression and hemodynamic compromise including:
low cardiac output syndrome
cardiogenic shock
potentially pathologically characterized by diffuse inflammatory infiltrates
chronic myocarditis: ongoing chronic myocardial inflammation with myocardial fibrosis in the setting of nondilated or mildly dilated arrhythmogenic cardiomyopathy
chronic inflammatory cardiomyopathy: persistent or chronic inflammatory process (symptom onset >1 month) associated with cardiac dysfunction and remodeling, either as a dilated or non-dilated clinical phenotype and possibly accompanied by an arrhythmogenic substrate
drug-induced myocarditis: caused by direct drug-toxicity e.g. cocaine use
eosinophilic myocarditis: myocardial inflammation with an eosinophilic infiltrate
giant-cell myocarditis: myocarditis histologically characterized by myocardial infiltration of large multinuclear giant cells
hypersensitivity myocarditis or allergic myocarditis: usually caused by an abnormal reaction to drugs and characterized by an eosinophilic infiltrate
immune-mediated myocarditis: caused by immune mechanisms e.g. autoimmune disease or heart transplant rejection
immune checkpoint-associated myocarditis: a special form of immune-mediated myocarditis associated with the use of immune checkpoint inhibitors
lymphocytic myocarditis: characterized by a lymphocytic infiltrate that is small mononuclear cells
sarcoidotic myocarditis: acute myocarditis in association with sarcoidosis – see: cardiac sarcoidosis
virus-induced myocarditis: probably or definitely related to viral infection, includes both virus-mediated and virus-triggered myocarditis
virus-mediated myocarditis: related to viral infection with demonstration of the viral genome in the myocardium
virus-triggered myocarditis: lymphocytic myocarditis triggered by common viruses, without the evidence of a viral genome within the heart muscle
Diagnosis
Endomyocardial biopsy is considered the gold standard of diagnosis, although it is subject to sampling error and there is a risk of perforation or tamponade. It is graded according to the Dallas criteria, with gradations of myocarditis, borderline myocarditis, and no myocarditis.
A typical appearance of myocarditis on MRI in the correct clinical setting may obviate biopsy.
Clinical presentation
Clinical presentation is variable in severity, ranging from asymptomatic to cardiogenic shock, but it typically is associated with other viral symptoms, including fever and malaise. It typically occurs 7-10 days after the onset of the systemic illness.
Chest pain may occur, in a variety of typical and atypical presentations.
Lab values are typically non-specific, with increased ESR and leukocytosis. Creatine kinase, CK-MB, and troponins may be elevated. A viral titer may be positive.
ECG
Commonly sought due to the clinical presentation, but demonstrates poor sensitivity. Findings include:
-
sinus tachycardia
non-specific, most common overall electrocardiographic manifestation
concave, diffuse ST-segment elevation
-
interventricular conduction delays
right bundle branch block common in acute Chagas myocarditis
-
prolongation of the QRS complex duration (>0.12 seconds)
poor prognostic factor 5
Pathology
Myocarditis has several etiologies. Inflammation from viral etiologies is thought to be caused both by direct cellular damage by the infectious agent and also by involvement by the host's immune system.
Etiology
Infectious etiologies
viral (most common etiology): e.g. Coxsackievirus, Echovirus, arbovirus
bacterial, e.g. Corynebacterium diphtheriae, Streptococcus pyogenes, Staphylococcus aureus, Borrelia burgdorferi
fungal, e.g. Candida spp.
parasites, e.g. Trypanosoma cruzi
Non-infectious etiologies
-
drugs
antibiotics
antituberculous agents
antiseizure medications
anti-inflammatories
diuretics
non-prescription/recreational drugs
Covid-19 vaccines 6
radiation
transplant rejection
-
systemic disease
Markers
Although non-specific, cardiac creatine kinase (CK) and troponins I, T and C (TnI, TnT and TnC) are elevated.
Classification
Myocarditis is classified into four categories based on the clinical and pathologic presentation: fulminant, acute, chronic active, and chronic persistent.
Radiographic features
Ultrasound
Echocardiography
Primarily useful to exclude alternative diagnoses which present similarly, including ischemic heart disease, and evaluate for the presence or absence of a pericardial effusion (and potential tamponade physiology). Findings common in myocarditis include 8:
global left ventricular systolic dysfunction
regional wall motion abnormalities
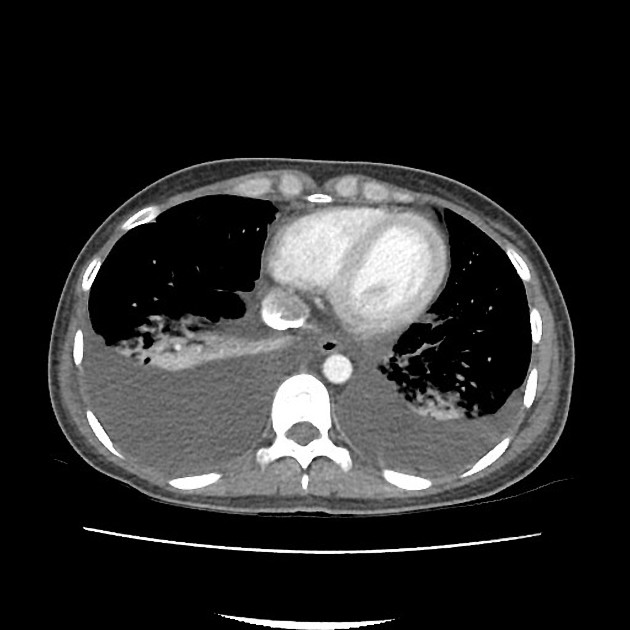
CT
Not always useful but some case reports describe certain features that can be helpful such as delayed myocardial enhancement (i.e. similar to MRI) with iodinated contrast 9,10.
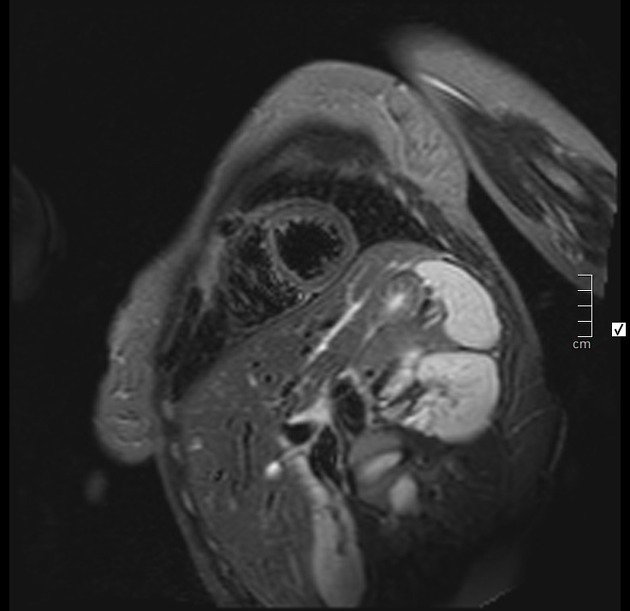
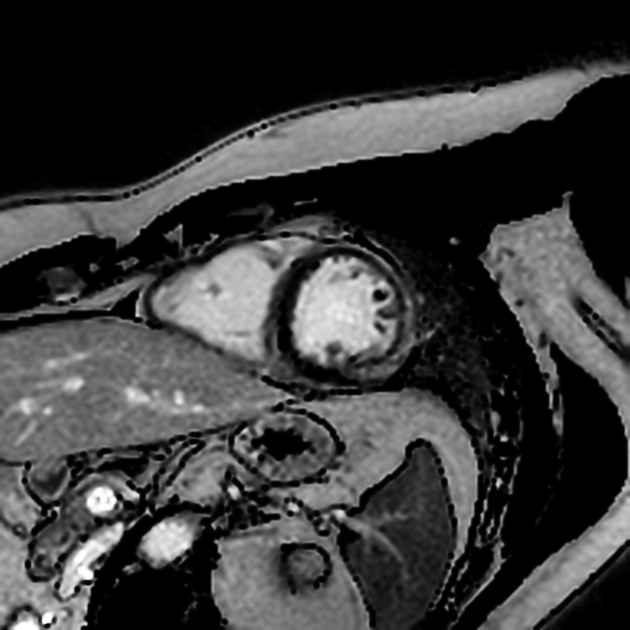
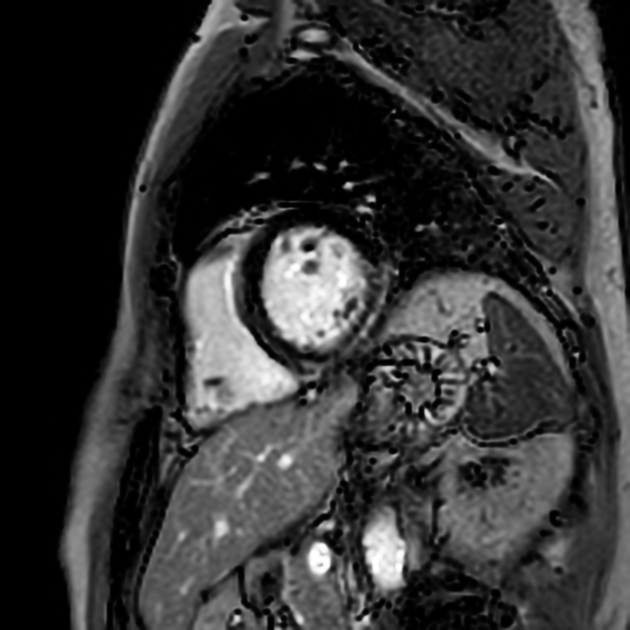
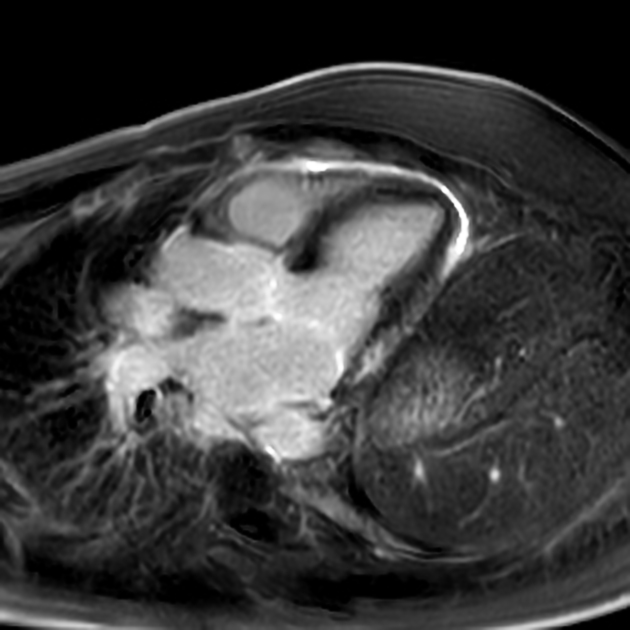
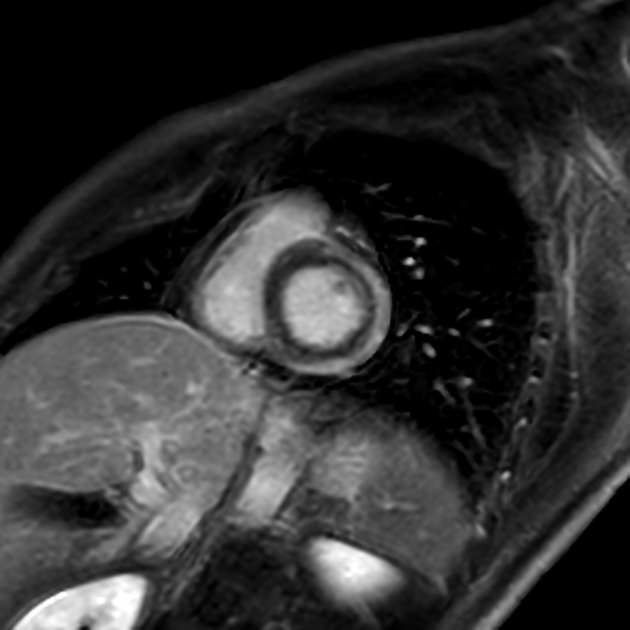
MRI
-
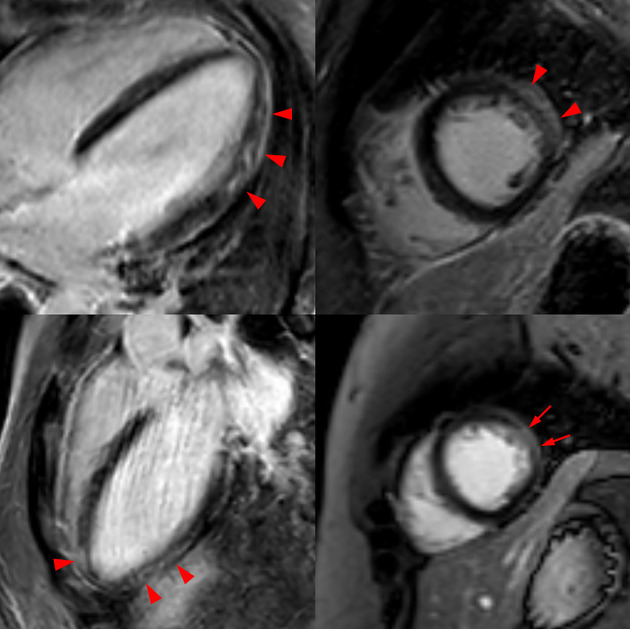
cine SSFP
regional or global wall motion abnormalities are common but nonspecific (biventricular wall motion abnormality, however, is the main predictor of death or transplantation)
pericardial effusion is reported in ~45% (range 32-57%) of patients with myocarditis
-
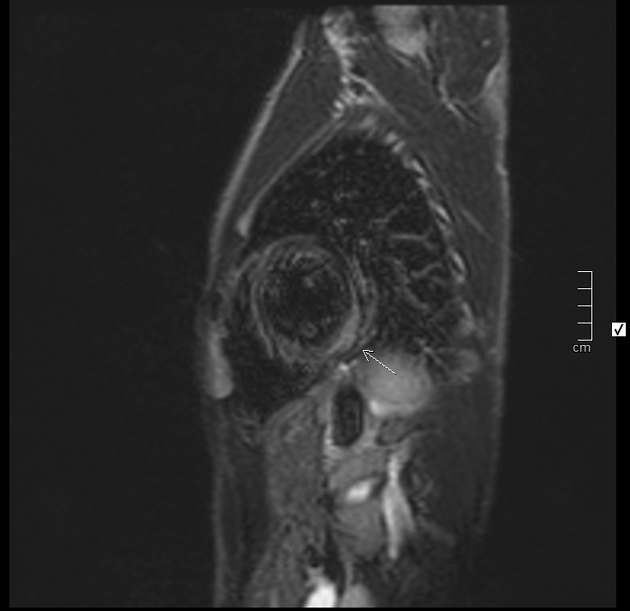
T2 black blood
T2 myocardial hyperintensity is compatible with edema
T2 hyperintensity may be global and difficult to detect
-
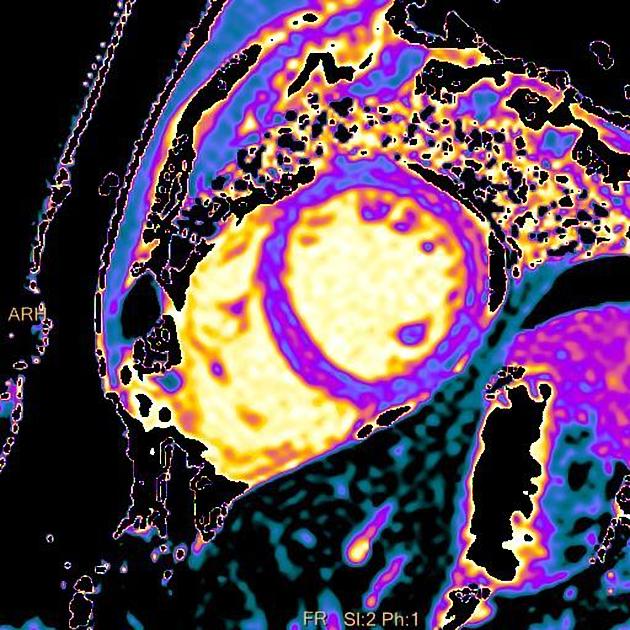
early gadolinium enhancement
regional vasodilatation and increased blood volume due to the inflammation in myocarditis causes early postcontrast enhancement
-
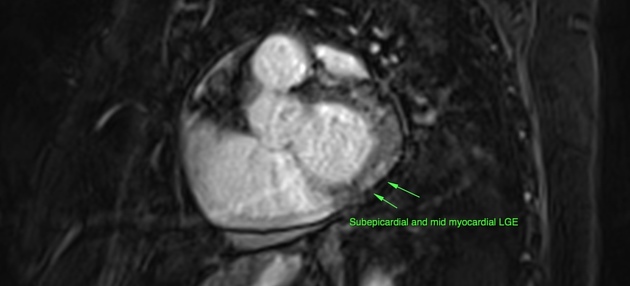
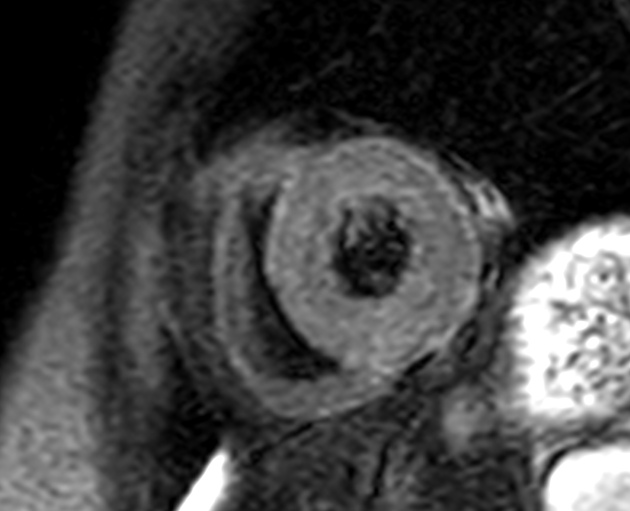
late gadolinium enhancement
late gadolinium enhancement in myocarditis is an indication of irreversible myocardial necrosis and fibrosis.
distribution of enhancement is variable but classically involves the subepicardial myocardium (mid-interventricular and focal transmural patterns are also possible)
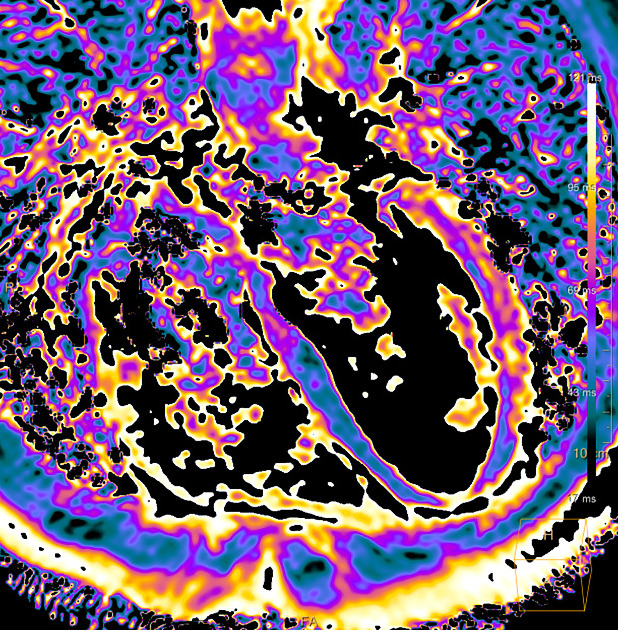
Lake Louise Criteria 2018
The original Lake Louise Criteria 14 were updated in 2018. The following two main criteria (T1 and T2 criteria) have to be fulfilled for the diagnosis of acute myocarditis 15:
-
T2-weighted: any of the following
standard T2 sequences: regional high signal
standard T2 sequences: global signal intensity ratio (myocardium/skeletal muscle) ≥2
T2 mapping: increased T2 relaxation times
-
T1-weighted: any of the following
late enhancement imaging: non-ischemic (subepicardial or mid-myocardial) late enhancement
native T1 mapping: increased T1 relaxation times or extracellular volume
-
supportive criteria:
signs of pericarditis: effusion or pericardial late enhancement
regional or global wall motion abnormalities
History and etymology
Inflammation of the heart was first described by the French physician Jean Baptiste Senac (1693-1770) in his work ‘Traité de la structure du cœur, de son action et de ses maladies’ 17. The term ‘myocarditis’ however was introduced later by the German physician and medical writer Joseph Sobernheim in 1837 18,19.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.