Myxoid soft tissue tumours are diversified group tumours of mesenchymal origin with a mucoid or myxoid extracellular matrix, which can be benign or malignant 1-3.
On this page:
Epidemiology
Incidence depends entirely on the specific tumour with intramuscular myxoma being the most common 2,3 from the benign lesions. Aggressive angiomyxoma is a locally aggressive benign variant affecting mostly women 2,3. Fairly frequent malignant myxoid tumours include myxoid liposarcoma making up 20-50% of all liposarcomas 3, myxofibrosarcoma, formerly known as myxoid malignant fibrous histiocytoma, which is a common malignant soft tissue tumour in the elderly 3.
Myxoid chondrosarcomas, ossifying fibromyxoid tumours, low-grade fibromyxoid sarcoma and myxoinflammatory fibroblastic sarcomas are rare variants from the malignant group 2,3 and superficial angiomyxoma, myxolipoma and acral fibromyxoma are rare benign myxoid tumours 2.
Clinical presentation
Depending on the entity most patients will present with a lump or other painless soft tissue mass somewhere in their extremities or trunk, or they are entirely asymptomatic. Some tumours as extraskeletal myxoid chondrosarcomas or aggressive angiomyxomas can cause pain and tenderness the latter in the perineum 2,3.
Diagnosis
The diagnosis is established by histological evidence of a myxoid extracellular matrix.
Pathology
Myxoid tumours produce a myxoid extracellular matrix, which is quite heterogeneous among different tumours basically composed of different proteoglycans and glycosaminoglycans (GAGs) 1-4 of which none is specific for a lesion and hyaluronic acid is the most common 4. The myxoid extracellular matrix itself is a histological feature in diverse physiological and pathological conditions 6 and is also found in mesenchymal and epithelial tumours. It is often only a secondary phenomenon in the latter and is more often an intrinsic part of the respective mesenchymal soft tissue tumour 4.
Macroscopic, microscopic appearances markers and genetics will depend on each separate entity.
Location
Most myxoid soft tissue tumours will be found in the extremities and less often in the trunk 2,3. Intramuscular myxomas will most often occur intramuscularly and in rare occasions intermuscular or subcutaneous; the thigh is the most commonly affected extremity 2,5.
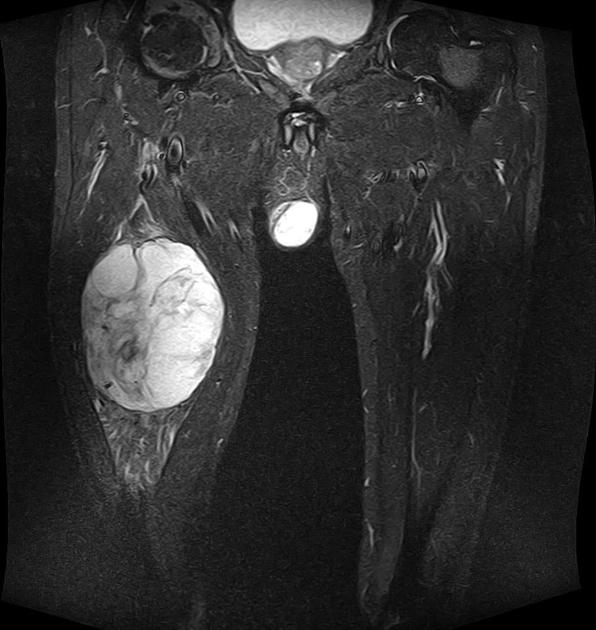
Aggressive angiomyxomas are typically found in the perineal area of women in their 20s to 40s 2,3.
Myxoid liposarcomas and extraskeletal myxoid chondrosarcomas are typically located within the lower extremities hips, buttocks and trunk 2,6.
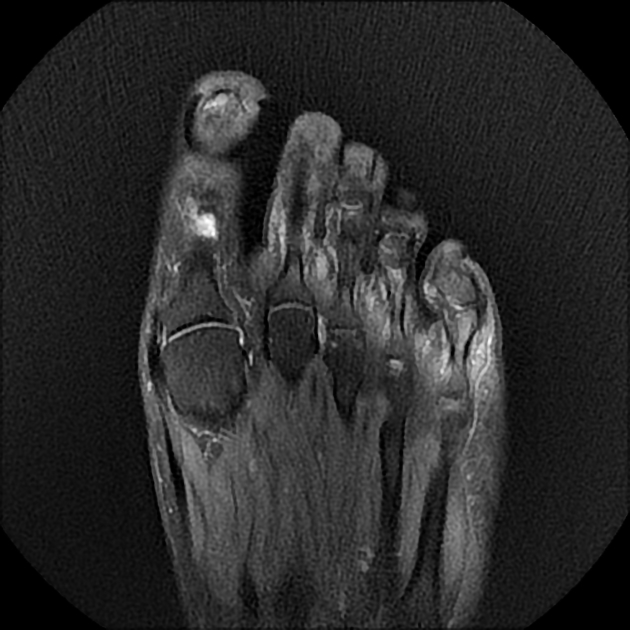
Myxoinflammatory fibroblastic sarcoma and acral fibromyxoma typically involve the distal extremities and the subcutaneous tissues 2.
Classification
The classification of soft tissue tumours was published in the WHO classification 2002, revised 2013 and is mainly founded on clinicopathological and cytogenetic/molecular variations.
A simplified classification for myxoid soft tissue tumours was proposed by Baheti et al. and lists the most important benign and malignant neoplasms 2:
Benign myxoid soft tissue tumours
- intramuscular myxoma
- juxta-articular myxoma
- aggressive angiomyxoma
- superficial angiomyxoma
- acral fibromyxoma
- dermal nerve sheath myxoma
Malignant myxoid soft tissue tumours
- myxoid liposarcoma
- myxoid pleomorphic liposarcoma
- myxofibrosarcoma
- low-grade fibromyxoid sarcoma
- extraskeletal myxoid chondrosarcoma
- ossifying fibromyxoid tumour
- myxoinflammatory fibroblastic sarcoma (MIFS)
Radiographic features
A common feature of all myxoid tumours is their high water content 1-4. Most myxoid tumours will also show a certain heterogeneity. Other features will depend on the respective tumour and will show other features as perilesional fat and/or oedema, fatty components, ossifications, calcifications subcutaneous or dermal involvement. Whereas most myxoid soft tissue tumours are well defined, myxofibrosarcomas often have an ill-defined appearance 2.
Plain radiograph
Most myxoid tumours of the soft tissue will not be evident on radiographs unless large, then will be evident as soft tissue swelling.
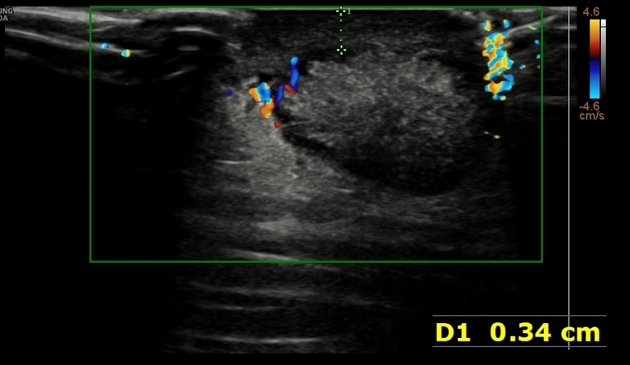
Ultrasound
Myxoid lesions will usually be hypoechoic to anechoic in ultrasound 2,3.
CT
Usually hypodense lesions with densities higher than water 2,3, but definitely less than muscle 2.
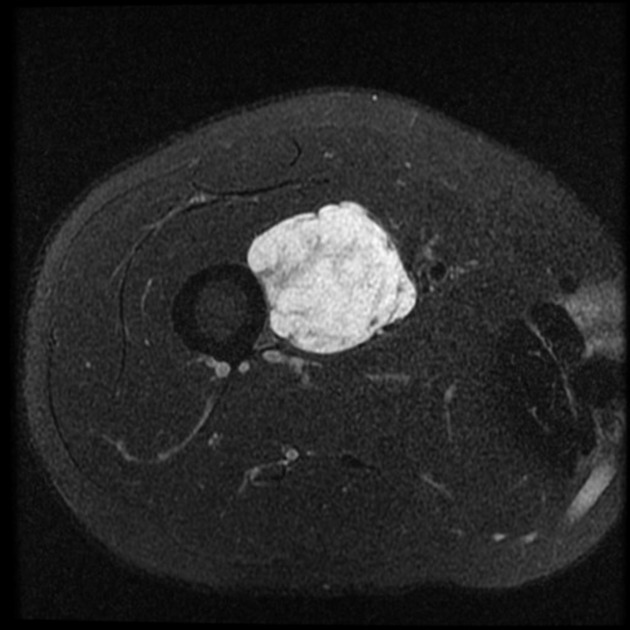
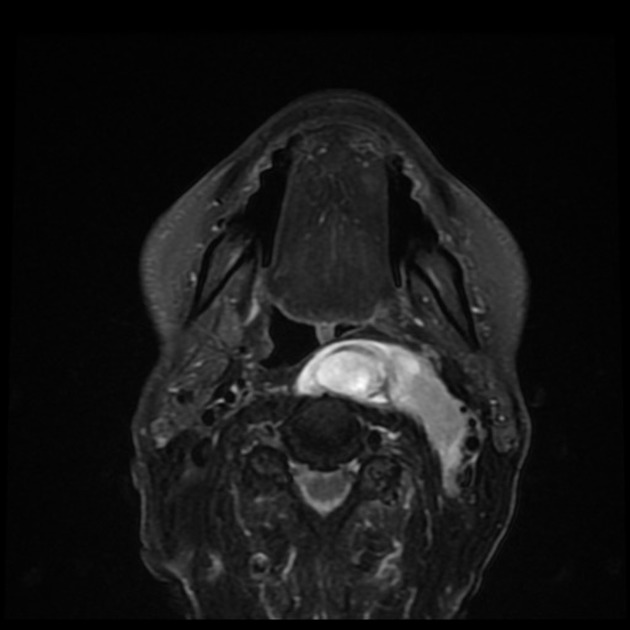
MRI
Some well-defined tumours show perilesional oedema or fat 2.
Signal characteristics
- T1: hypointense to muscle
- T2: hyperintense
- T1 C+: variable patterns of enhancement exist
Treatment and prognosis
Will entirely depend on the underlying tumour.
Malignant tumours and local aggressive tumours as the intramuscular myxoma and aggressive angiomyxoma will mostly be excised with margins 2,3 and again depending on the respective lesion might require further adjuvant or neoadjuvant chemotherapy or chemoradiation 2,3.
For most other benign tumours therapy will depend on symptoms 2.
History and etymology
The term myxosarcoma was introduced by Bryant, which he defined as “mucous transformation of malignant round cell sarcomas usually attacking the omentum and skin” 4.
Müller described the myxoid matrix 1838 as 'collonema', in greek “κολλα” stands for glue and described it further as an “odd gelatinous tumour of soft gelatiniform tissue, which trembles when touched” 4.
The term “myxoma” was then introduced by Rudolph Virchow in Cellularpathologie, 1858. He used it to describe a myxoid soft tissue tumour, which he compared with the jelly-like structure of the umbilical cord 4.
Differential diagnosis
The differential diagnosis includes many tumour-like myxoid lesions e.g. ganglion cysts and synovial cysts peripheral nerve sheath tumours including neurofibromas and schwannomas 2,3 and other benign and malignant soft tissue tumours 2.
- ganglion cysts / synovial cysts
- peripheral nerve sheath tumours
- rhabdomyoma/rhabdomyosarcoma
- lymphangioma
- chronic haematoma
Practical points
The finding of a T1 hypointense and T2 hyperintense lesion of the musculoskeletal system, which enhances after contrast and spares the visceral organs, is indicative of a myxoid origin 2.
An approach to these tumours is to look at the site of involvement and the patient's age 2.
A tumour with a swirling pattern of the perineal region without the involvement of the viscera in a woman in her 3rd or 4th decade might reflect an aggressive angiomyxoma, if the lesion is intramuscular and well defined an intramuscular myxoma is very likely. If a myxoid lesion is located in the extremities of a patient in the 6th decade of life and shows an ill-defined appearance a myxofibrosarcoma should be considered. If it is located in the distal extremities with subcutaneous involvement one should think of myxoinflammatory fibroblastic sarcoma (MIFS). The presence of fatty components should suggest a myxoid liposarcoma. Are there ossifications present? – think of ossifying fibromyxoid tumours and noncalcified large lobulated tumours in the proximal lower extremities or limb-girdle regions should rise the thought of extraskeletal myxoid chondrosarcoma 2.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.