Oesophageal atresia refers to an absence in the continuity of the oesophagus due to an inappropriate division of the primitive foregut into the trachea and oesophagus. This is the most common congenital anomaly of the oesophagus.
On this page:
Epidemiology
It is thought to occur in ~1:3000-4500 live births 3.
Associations
Oesophageal atresias are frequently associated with various other anomalies (50-75% of cases). They include
-
other intestinal atresias
VACTERL association inclusive of congenital cardiac anomalies
-
increased incidence of chromosomal anomalies such as
Clinical presentation
Oesophageal atresia may be suspected on antenatal ultrasound (see below) or in the neonate due to inability to swallow saliva or milk, aspiration during early feedings, or failure to pass a nasogastric tube into the stomach successfully.
Pathology
It results from a failure of the primitive foregut to divide into the trachea anteriorly and the oesophagus posteriorly. This usually occurs at around the 4th week of gestation.
General pathogenesis includes teratogenic effects caused by early pregnancy use of antithyroid drugs 7
Genetics
Most cases have a sporadic occurrence 6.
Subtypes
It is frequently associated with a tracheo-oesophageal fistula. As such, the types of oesophageal atresia / tracheo-oesophageal fistula can be divided into 4:
proximal atresia with distal fistula: 85%
isolated oesophageal atresia: 8-9%
isolated fistula (H-type): 4-6%
double fistula with intervening atresia: 1-2%
proximal fistula with distal atresia: 1%
See oesophageal atresia classification for further details.
Radiographic features
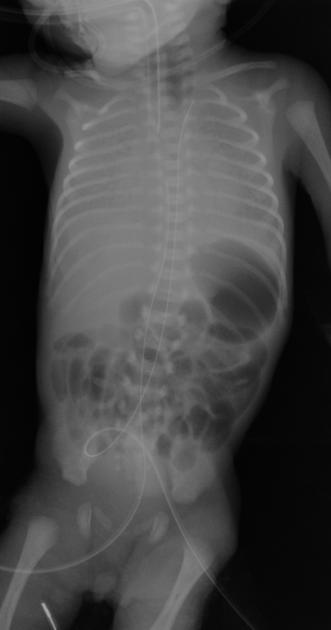
Plain radiograph
A chest/abdominal radiograph may show:
a dilated pharyngeal pouch
the presence of air in the stomach and bowel in the setting of oesophageal atresia implies that there is a distal fistula
if an oesophagogastric (feeding) tube insertion has been attempted this may show the tube blind looping and turning back at the upper thoracic part of the oesophagus or heading into the trachea and/or bronchial tree
Fluoroscopy
Contrast swallow may show contrast blindly ending and pooling in an oesophageal stump and/or may show evidence of the tracheo-oesophageal fistula. Fluoroscopy is particularly useful in demonstrating H-type fistula. A withdrawal oesophagogram is performed for a H-type fistula. The patient is positioned prone and a horizontal beam is used, contrast material is injected through the nasogastric tube into the distal oesophagus while the tube is slowly withdrawn under fluoroscopy 8. If the imaging study fails to locate the fistula while there is high suspicion then combined bronchoscopy and esophagoscopy is used 8. The gap between oesophageal pouches is determined by inserting a Higer dilator through a gastrostomy into the distal oesophagus and Repogle tube into the proximal pouch; both tubes are radiopaque 8.
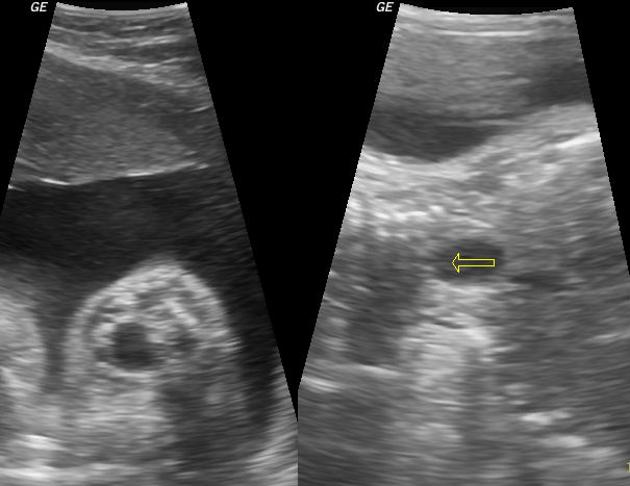
Ultrasound
non-specific but may not show the expected shape and position of the stomach
should be suspected if other VACTERL anomalies are seen
polyhydramnios may be present particularly in cases where there is no concurrent fistulation
the fetus may appear growth restricted
the subtypes without a tracheo-oesophageal fistula may be suspected in the context of persistent non-visualisation of the fetal stomach
CT
has been trialled for 3D detailed visualisation of anatomy but not part of routine investigation 3
Treatment and prognosis
Surgical intervention with a re-anastomosis can be attempted post-delivery. Methods of surgical intervention for oesophageal atresia would depend on the inter-pouch gap. The prognosis is variable depending on other associated anomalies.
Oesophageal strictures and anastomotic leak secondary to surgical correction of oesophageal atresia are known complications of the procedure and may require further surgical correction.















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.