Orbital infection is a relatively commonly encountered pathology.
It comprises of three main clinical entities with the most important distinction between that of orbital and periorbital cellulitis:
-
periorbital cellulitis (preseptal cellulitis) is limited to the soft tissues anterior to the orbital septum 1
often managed with oral antibiotics
-
orbital cellulitis (postseptal cellulitis) extends posteriorly to the orbital septum 1
a more serious condition requiring hospitalisation and parenteral antibiotics
complications such as intraorbital abscess formation may require surgical intervention
-
endophthalmitis involves an intraocular extension of infection
requires intraocular antibiotics
possible choroidal debridement or vitrectomy
On this page:
Epidemiology
Orbital infections represent more than half of primary orbital disease processes 2. These infections typically present in children and young adults but can affect any age group.
Clinical presentation
Pathology
Aetiology
Periorbital cellulitis often results from contiguous spread of an infection of the face, teeth, or ocular adnexa. Orbital cellulitis typically occurs as an extension of paranasal sinusitis 1. Endophthalmitis is most commonly secondary to ocular surgery or penetrating injury.
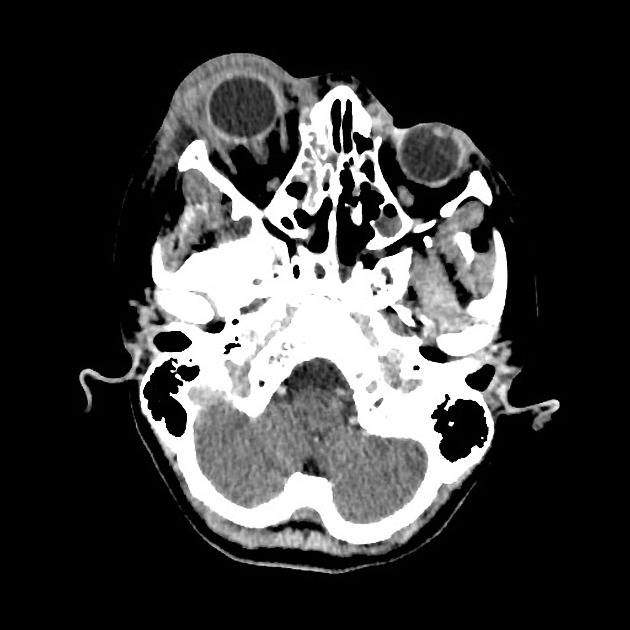
Radiographic features
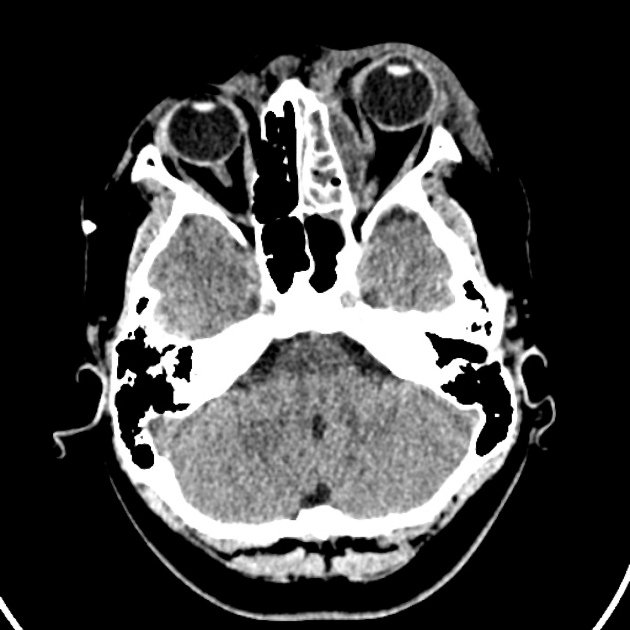
Urgent imaging is indicated to assess the anatomic extent of disease, including postseptal, cavernous sinus and intracranial involvement; evaluate for sources of contiguous spread, e.g. sinusitis or trauma; and identify orbital abscesses that require exploration and drainage 3. CT is the imaging investigation of choice as it is:
readily available at all hours and quick
ideal for assessing for underlying sinus disease
will identify a subperiosteal reaction or intracranial extension
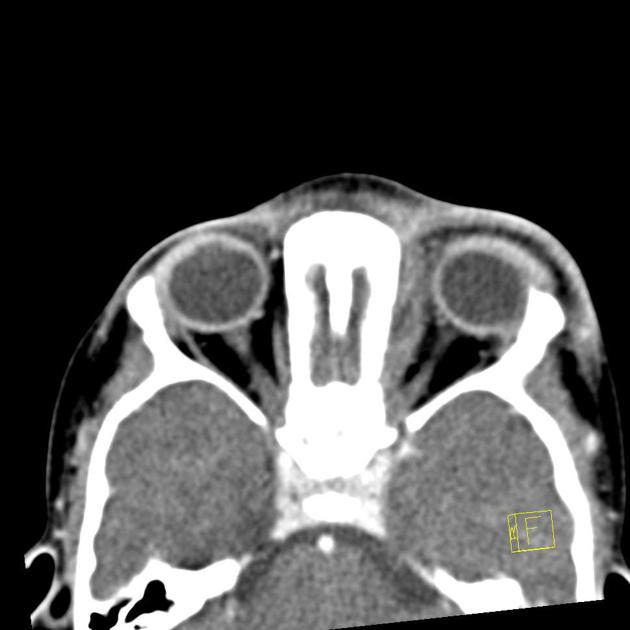
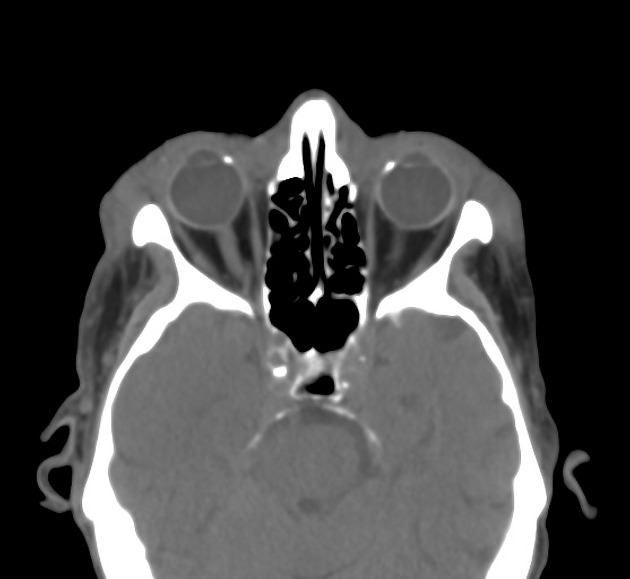
CT
Periorbital cellulitis
Diffuse soft-tissue thickening and areas of enhancement anterior to the orbital septum are seen in periorbital cellulitis. It is very difficult to differentiate between preseptal oedema and periorbital cellulitis on CT 4.
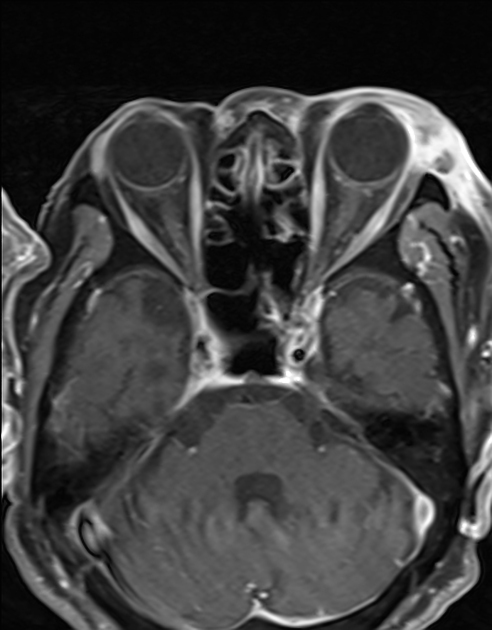
Orbital cellulitis
poor definition of orbital planes
inflammatory stranding in the intraconal fat
intraconal or extraconal soft tissue mass
oedema of the extraocular muscles
intraorbital abscess
Endophthalmitis
Findings are often non-specific, though choroidal enhancement may be seen in the early phases.
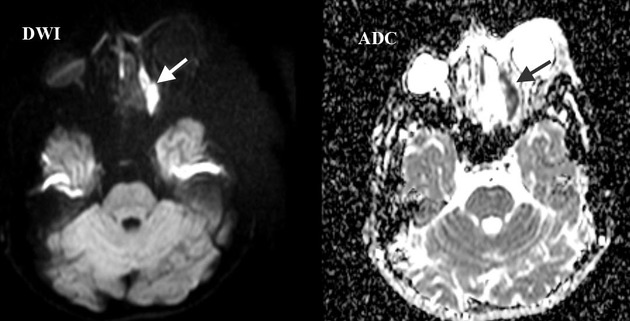
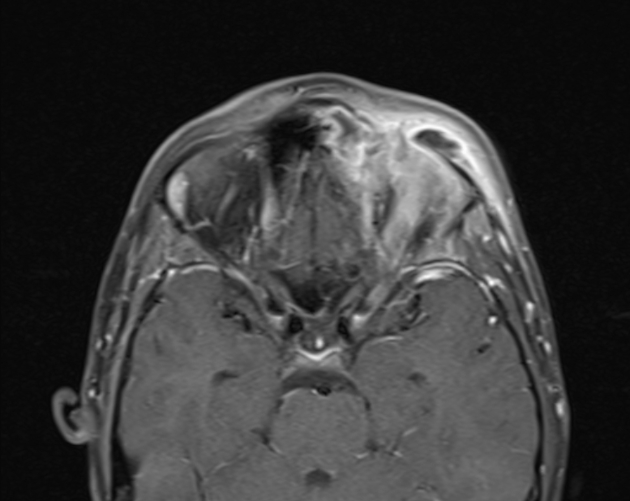
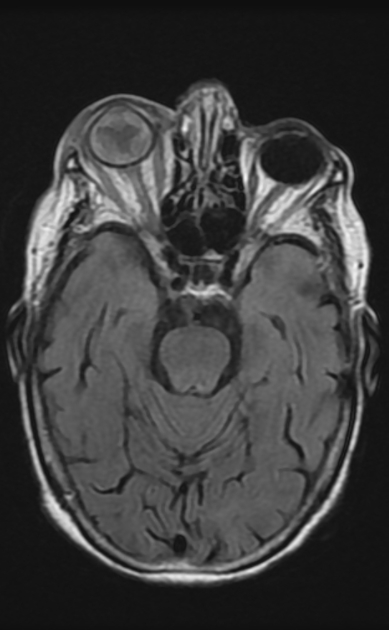
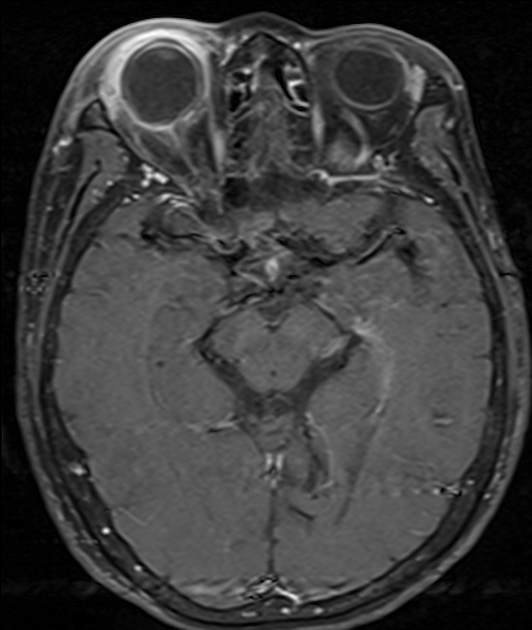
MRI
Rarely performed, as not usually necessary. Like CT, it will identify a subperiosteal abscess as:
T1: low signal
T2: high signal
DWI/ADC: diffusion restriction
T1 + C: rim enhancement
MRI may occasionally have a role in diagnosing endophthalmitis since the presentation can often be non-specific. Key findings include:
T2 FLAIR: high signal
DWI/ADC: diffusion restriction in the affected globe
Treatment and prognosis
Periorbital cellulitis is treated with oral antibiotics. Orbital cellulitis is treated with intravenous antibiotics. However, if a subperiosteal abscess is present, surgical drainage may be necessary 1.
Complications
Complications of orbital cellulitis include 1:
loss of vision









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.