Pancoast tumour, also known as superior sulcus tumour, refers to a relatively uncommon situation where a primary lung cancer arises in the lung apex and invades the surrounding soft tissues. Classically, a Pancoast syndrome results, but this is only seen in one-quarter of cases.
On this page:
Terminology
The term superior pulmonary sulcus is now discouraged, both as a discrete anatomical entity and as a site for the origin of malignancy. It is an unhelpful term, not least because most formal anatomical texts do not even mention it as a structure. Moreover, there is no consistent usage in the literature as to what it actually refers to 12. Using the term "superior sulcus tumour" is imprecise and unneeded, as in all situations a 'lung apical tumour' would suffice as an alternative. Notwithstanding the above, the term superior sulcus tumour is still seen in the radiological, medical and surgical literature. For the remainder of the article whenever Pancoast tumour or apical lung tumour is mentioned, the term superior sulcus tumour can be substituted, although we discourage its use.
Definitions vary from author to author, with some only referring to Pancoast tumours if the histology is a non-small cell lung cancer (NSCLC), and treating other apical tumours separately (even though any apical malignancy can cause Pancoast syndrome) 7; and some only referring to Pancoast tumours if they have presented with Pancoast syndrome and call the rest apical tumours. Others use the term apical tumour and Pancoast tumour interchangeably but limit the use to lung cancers, while others include all tumours that involve the thoracic apex (whether or not they arise from the lung).
For the sake of simplicity, we have taken the middle road. For this article pulmonary apex tumour and Pancoast tumour are used interchangeably to refer to a primary lung cancer with an apical pulmonary origin.
Epidemiology
Pancoast tumours account for 3-5% of all lung cancers and have similar demographics to other lung cancers 5,8.
Clinical presentation
Although classically apical lung tumours present with Pancoast syndrome, this is only the case in approximately 25% of cases 1. The missing element is usually Horner syndrome.
The most common symptoms at presentation are chest and/or shoulder pain, with arm pain being also common. Weight loss is frequently present 5.
Pathology
Apical lung tumours are usually non-small cell lung cancers (NSCLC). The most common histology encountered historically in this region were squamous cell carcinomas 6,7, however, in keeping with the overall shift in frequency, pulmonary adenocarcinomas are now more frequently identified 8.
Radiographic features
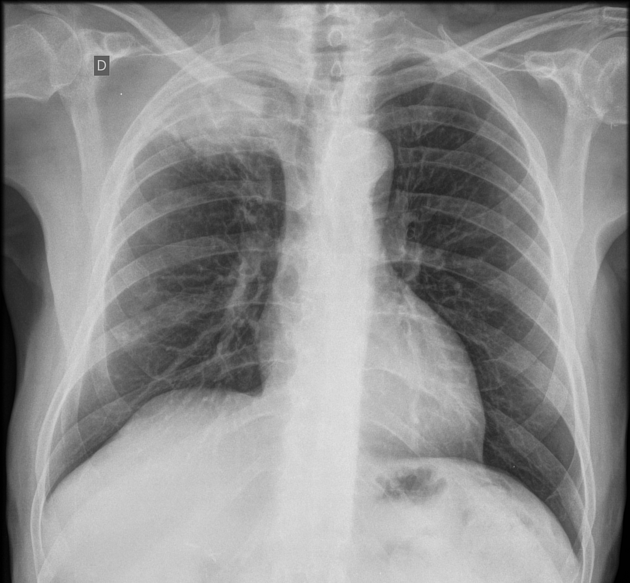
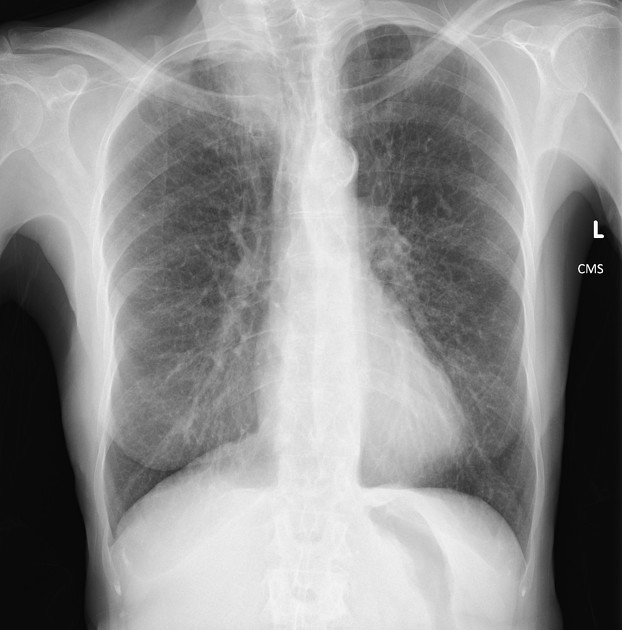
Plain radiograph
Plain films demonstrate a soft tissue opacity at the apex of the lung. Occasionally rib involvement or extension into the supraclavicular fossa may be evident. Lordotic views may be helpful.
Ultrasound
The role of ultrasound is limited, but it may be useful in aiding percutaneous biopsy as it can visualise the external component of the tumour via an intercostal or supraclavicular acoustic window 3.
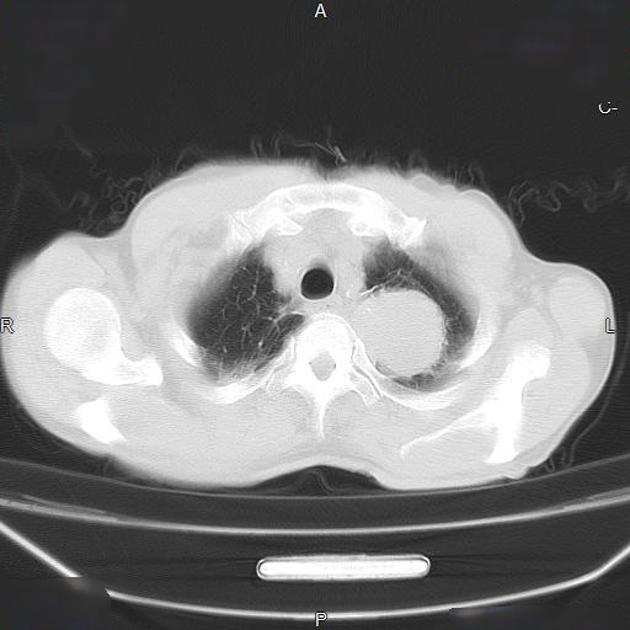
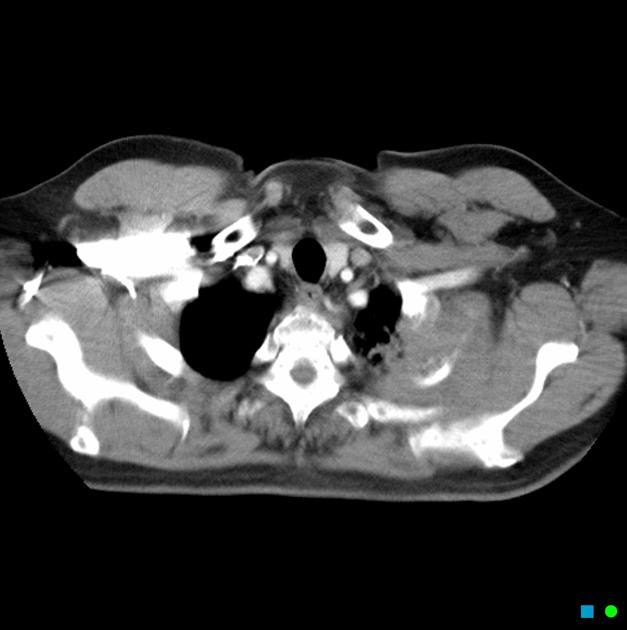
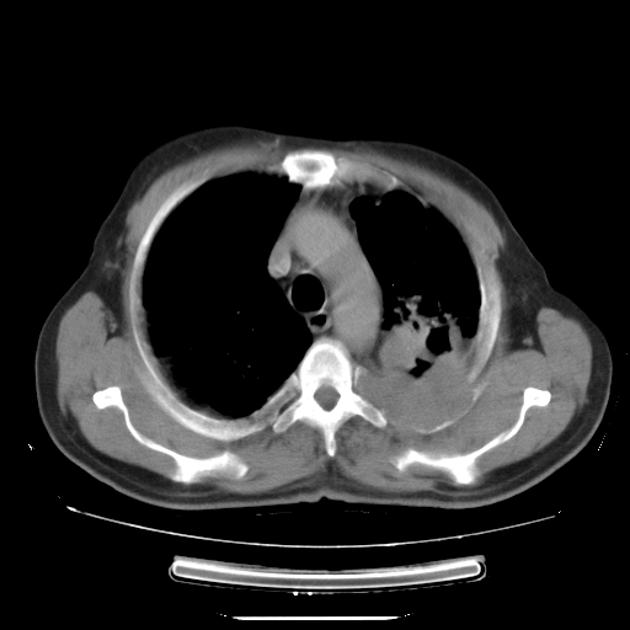
CT
Although, as is the case with lung cancer at other locations, CT is the workhorse for diagnosis, it has poor sensitivity (60%) and specificity (65%) for accurate local staging 7. It is, however, excellent at identifying bony involvement.
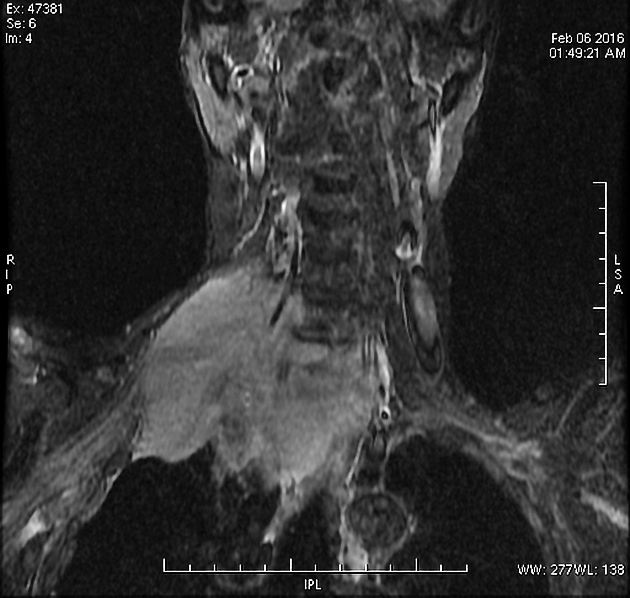
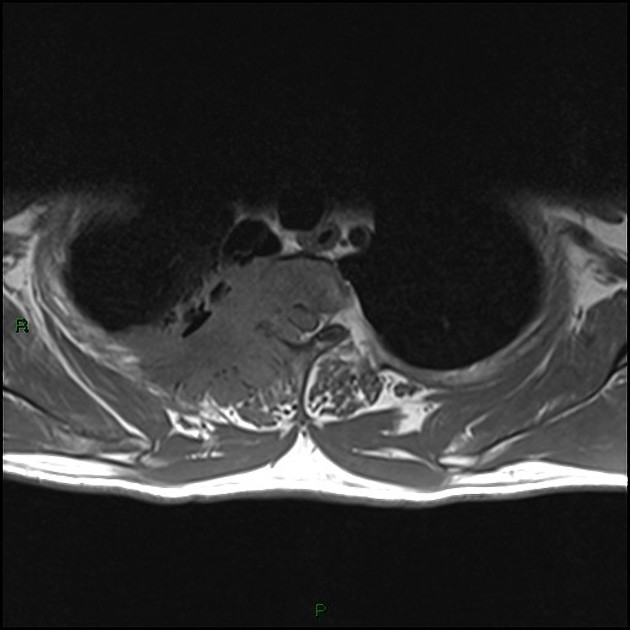
MRI
MRI is helpful in the assessment of pulmonary apical tumours due to its excellent demonstration of soft-tissue involvement and is far more sensitive (88%) and specific (100%) for local staging 7.
Careful assessment of the brachial plexus is important as the involvement of more than the lower trunk, or C8 nerve root, is usually considered inoperable 7.
The anatomy lends itself particularly to imaging in the coronal and sagittal plane, and the T1 sagittal images offer most of the required information 2,8.
PET-CT
As for lung cancers in general, it is useful for assessing nodal and distant metastases at the baseline staging. For Pancoast in particular, PET-CT permits an accurate delineation of the gross tumour volume, which will be essential for the radiation treatment planning 8.
Treatment and prognosis
Treatment depends crucially on the extent of involvement notably through the apex, as these lesions usually involve the brachial plexus and subclavian vessels. In such lesions, radiotherapy is typically administered in an attempt to downstage the tumour sufficiently to allow for attempted resection 2.
Much controversy nonetheless exists over exact inclusion and exclusion criteria for surgery and the timing and administration of radiotherapy and chemotherapy.
Despite advances in management, prognosis remains poor with an overall 5-year survival of only 36%. Complete resection is the most important factor in determining survival 5:
complete resection achieved - 45% 5-year survival
incomplete resection only - 0% 5-year survival
History and etymology
Pancoast syndrome as a result of superior sulcus tumours was described in some publications (Hare 1838 and Ciuffini in 1911) before Pancoast reported it using the term 'superior pulmonary sulcus tumour' in 1924 5,8,9:
Edward Selleck Hare (1812-1838), British physician, who died tragically at the age of 26 years from typhus 10
Publio Ciuffini, Italian physician: it is stated elsewhere that Ciuffini, a bona fide Italian physician of the early 20th century, described this entity in 1911, however an original reference remains elusive
Henry Khunrath Pancoast (1875-1939) 11, American radiologist
Differential diagnosis
General imaging differential considerations include:
chest wall metastases
apical pleural thickening secondary to e.g. previous pulmonary tuberculosis
In addition a number of plain film mimics should be considered, including:
vascular lesions: e.g. carotid pseudoaneurysm 4













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.