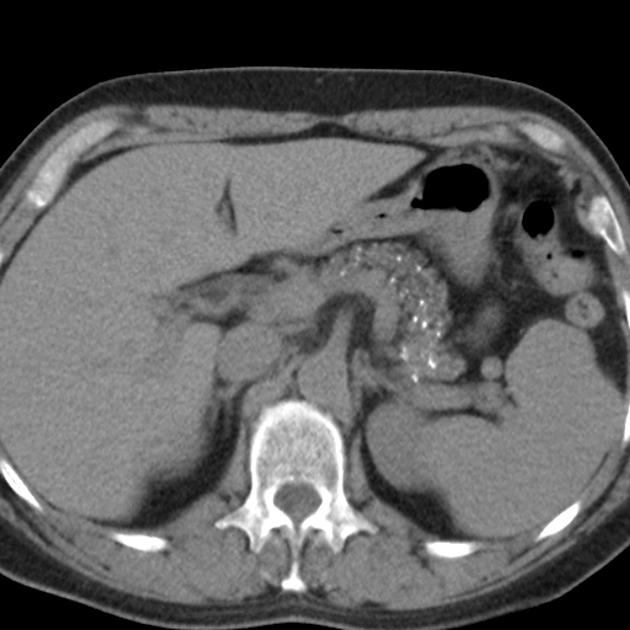
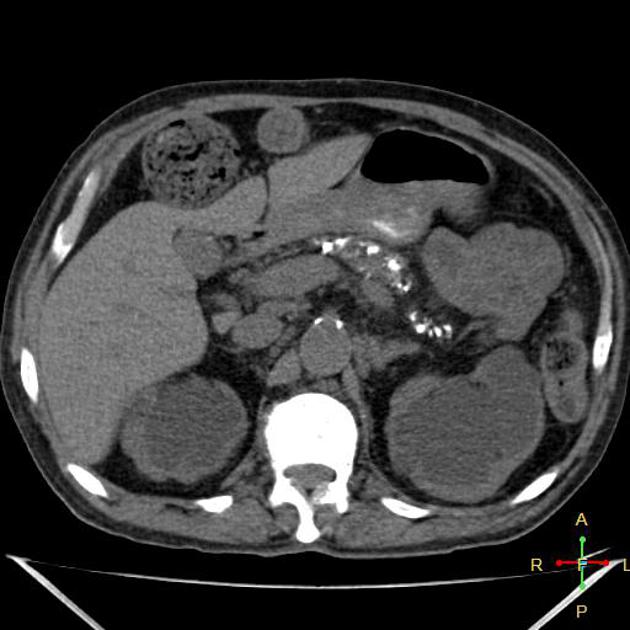
Pancreatic calcifications can arise from many aetiologies.
Punctate intraductal calcifications
-
-
alcoholic pancreatitis (20-40%) 2
intraductal, numerous, small, irregular
preponderant cause of diffuse pancreatic intraductal calcification
-
much less commonly associated with calcifications
-
most also have nephrocalcinosis or urolithiasis (70%)
-
-
calcifications are common
manifest in the paediatric population
idiopathic: no underlying cause can be determined
Smaller intraductal calcifications
-
senile
usually in patients aged over 70 years
scattered
number of calcifications increase with age
cystic fibrosis: finely granular calcifications in smallest ducts in end stage disease with pancreatic failure
atherosclerotic calcifications
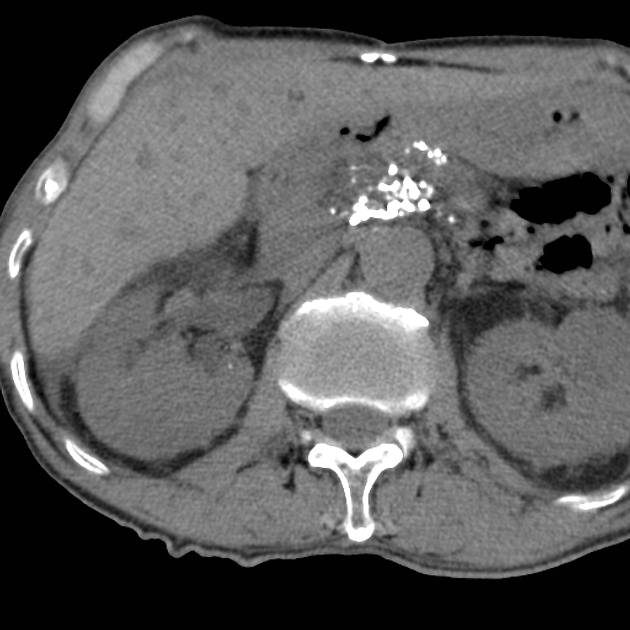
Larger intraductal calcifications
-
autosomal dominant 9% penetrance
large rounded shape
peaks at 5-17 years
gallstone migration
tropical pancreatitis: young patients in tropical countries
Dystrophic calcification
-
old insult
old infection
old infarction
old trauma
-
islet cell tumours: especially non-functional tumours; 20% islet cell tumours
-
calcified metastasis
colon
renal
-
mucinous (macrocystic) cystadenomas and carcinomas: mucus in tumour rarely calcifies; cysts >2 cm
serous (microcystic) cystadenomas and carcinomas: commonly calcify, characteristically as a central calcified scar with radiating calcified septations
intraductal papillary mucinous neoplasms: widened pancreatic duct extensive mucus
-
solid and pseudopapillary epithelial neoplasm
rare: in young women, commonly calcifies, characteristically punctate, peripheral calcifications
pancreatoblastoma: rare. ~ 20% calcify
cavernous lymphangioma / haemangioma (multiple phleboliths) 5
NB: adenocarcinomas of the pancreas do not generally calcify; rather, they typically engulf previously present adjacent calcifications.
Pancreatic calcification mimics
atherosclerosis of splenic artery and intrapancreatic arterioles
oral contrast in duodenal diverticula








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.