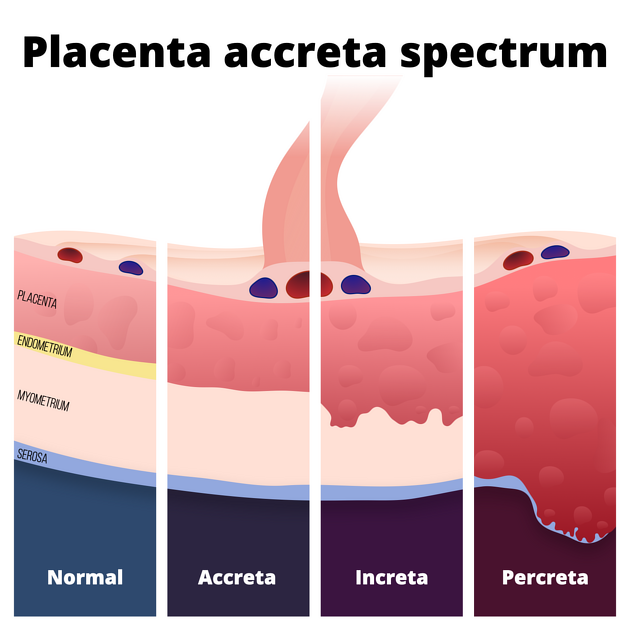
Placenta accreta is both the general term applied to abnormal placental adherence and also the condition seen at the milder end of the spectrum of abnormal placental adherence (placenta accreta spectrum disorders). This article focuses on the second, more specific definition.
In a placenta accreta, the placental villi extend beyond the confines of the endometrium and attach to the superficial aspect of the myometrium but without deep invasion.
The more severe end of the spectrum of abnormal placental villi adherence includes:
On this page:
Epidemiology
It is the most common form of placental invasion (~75% of cases). It is thought to occur in approximately 1 in 7000 pregnancies. The incidence is increasing due to the increased practice of caesarean sections. The combination of a previous caesarean section and an anterior placenta praevia should raise the possibility of a placenta accreta. This disease has maternal mortality of up to 7% depending on location.
Risk factors
Recognised primary risk factors for placenta accreta include:
prior caesarean section
previous uterine surgery
dilation and curettage
myomectomy
maternal age >35 years
multiparity
Pathology
The abnormal implantation is thought to result from a deficiency in the decidua basalis, in which the decidua is partially or completely replaced by loose connective tissue. In placenta accreta, chorionic villi and/or cytotrophoblasts directly attach to the myometrium with little or no intervening decidua.
Markers
elevated levels of α-fetoprotein
elevated levels of beta human chorionic gonadotropin (bHCG)
Radiographic features
Accurate prenatal diagnosis of placenta accreta is vital because this abnormality is an important cause of significant haemorrhage in the immediate post-delivery period with resultant maternal and fetal morbidity and mortality. However, the diagnosis is not often made prospectively.
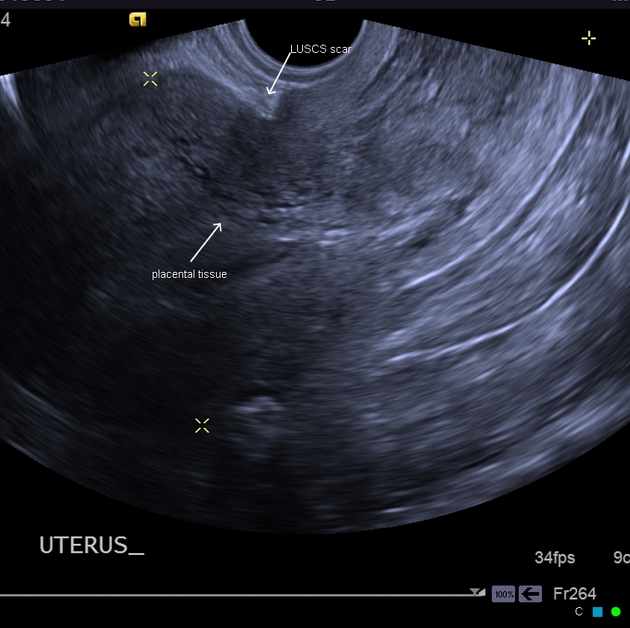
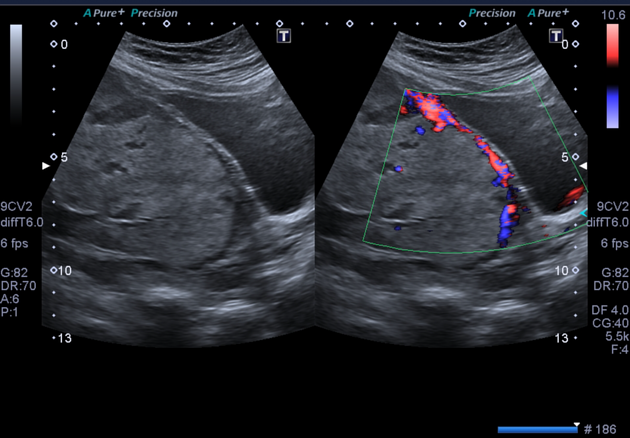
Ultrasound
According to one study 9, ultrasound has a sensitivity of 90%, a positive predictive value of 68%, and a negative predictive value of 98% for the diagnosis of placenta accreta.
Some features of placenta accreta on ultrasound are:
loss of the normal hypoechoic plane in the myometrium beneath the placental bed
presence of multiple placental lacunae
loss of the normal hyperechoic line separating the urinary bladder wall from the uterus
thinning of the myometrium to <1 mm
bulging of the placenta into surrounding organs adjacent to the uterus, causing a mass-like lesion protruding out from the uterine wall 10
When a placenta accreta occurs on the posterior or lateral walls of the uterus, it may be difficult to detect by ultrasound.
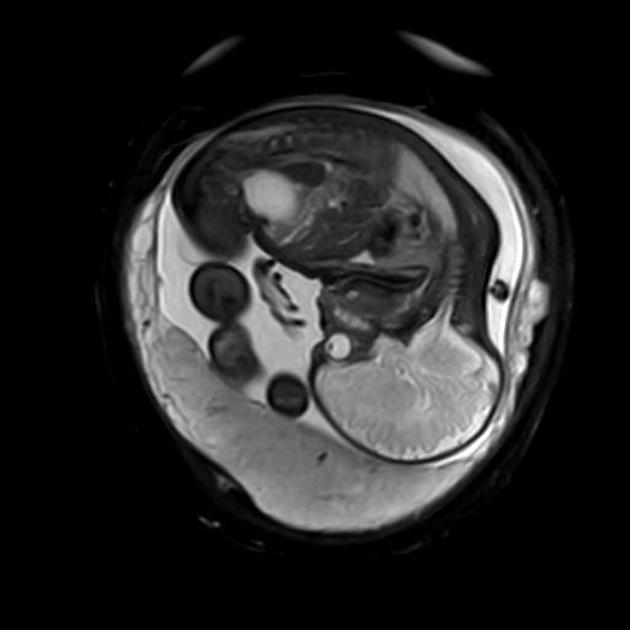
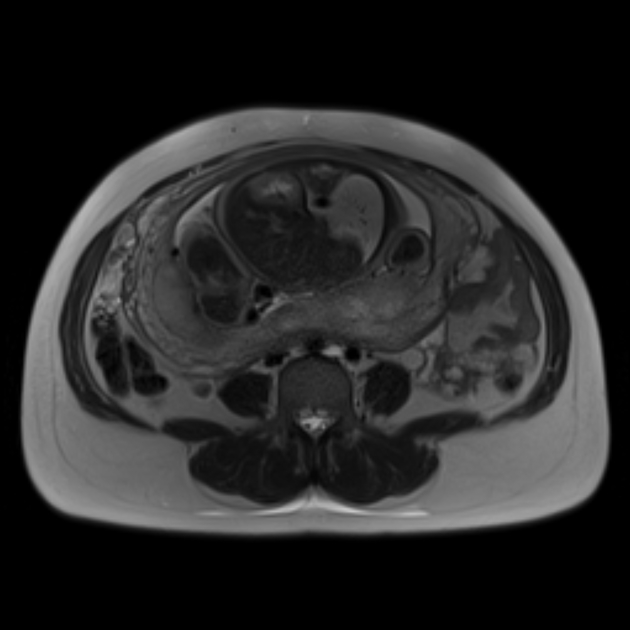
MRI
Magnetic resonance imaging has also been used to diagnose placenta accreta. Specific fast acquisition sequences (e.g. HASTE, true FISP) help to minimise fetal and maternal motion artifacts.
The demonstration of uterine bulging and loss of normal uterine contour.
-
T2
the mass is hyperintense and may be heterogeneous
T2 weighted imaging is useful in assessing for focal thinning of the myometrium and interruption of the junctional zone
Treatment and prognosis
A definitive treatment for placenta accreta consists of a hysterectomy with possible resection of adjacent organs if percreta is present. Placenta accreta is reported to be the most common indication for emergency peripartum hysterectomy.
In certain instances, however, conservative treatment may be used, especially if uterine preservation is desired. Conservative measures include curettage, oversewing of the placental bed, and ligation of the uterine arteries or the anterior divisions of the internal iliac arteries.
Complications
can progress to placenta increta, then placenta percreta on serial imaging
Differential diagnosis
subplacental hypervasculary: as placenta is highly vascularised, on evaluation with Doppler ultrasound subplacental hypervasculary may be seen in normal cases 11
adenomyosis: thick myometrium, cystic spaces and hypervascularity may mimick placental adhesion to myometrium but in placenta accreta spectrum, the myometrium is thin 11
Practical points
technical setting: with the PRF set >15 cm/s ,hypervascularity can be diagnosied more reliably 11






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.