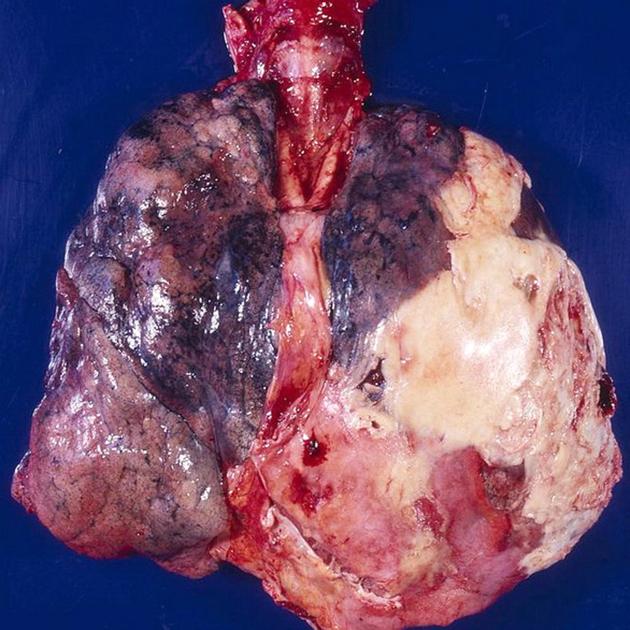
Pleural empyema refers to a collection of pus in the pleural cavity which may contain gas locules. Empyema is usually unilateral and most often occurs as a complication of pneumonia or perforated oesophagus. The thickened pleura demonstrates contrast enhancement and the visceral and parietal components separate around the collection causing the ‘split pleura sign’ 12.
On this page:
Epidemiology
Empyemas are usually the complication of another underlying abnormality, and thus demographics will follow those of the primary cause, e.g. pneumonia, subdiaphragmatic abscess, oesophageal perforation, etc.
Patients with HIV/AIDS are more likely to have pneumonia, and in turn are more likely to develop empyema, which may occur in >5% of cases of pneumonia 5.
Clinical presentation
Non-specific signs of infection and pneumonia with fever, leucocytosis and raised inflammatory markers.
Pathology
Microbiology
Offending organisms vary somewhat according to the age at which the empyema develops and the underlying cause. For parapneumonic empyemas the most frequent organisms are 7,9:
-
childhood
Pneumococcus
-
adults
penicillin-resistant Staphylococcus aureus
gram-negative bacteria
anaerobic bacteria: usually polymicrobial
In the setting of trauma or thoracic surgery, Staphylococcus aureus is usually involved 7.
Other uncommon causes include mycobacterial infection, resulting in tuberculous empyema.
Specific subtypes
Radiographic features
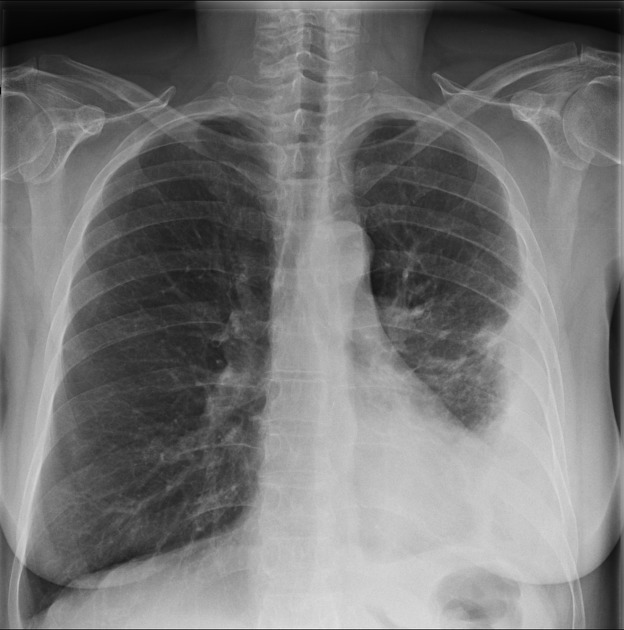
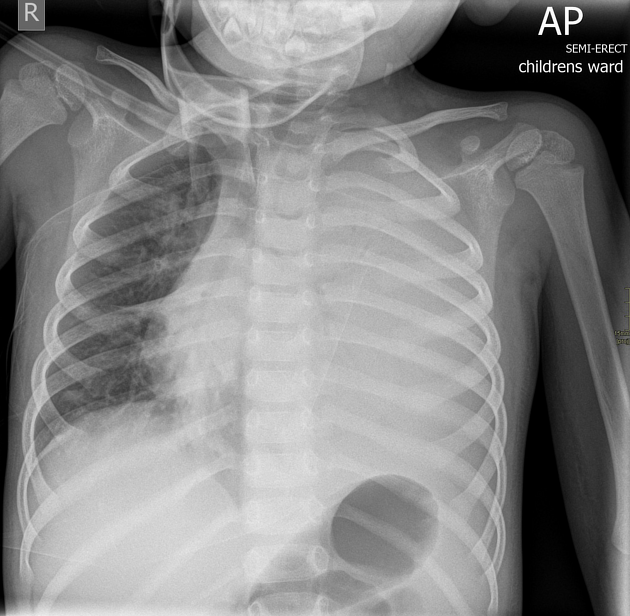
Plain radiograph
Empyema can resemble a pleural effusion or mimic a peripheral pulmonary abscess, although a number of features usually enable distinction between the two (see empyema vs lung abscess) 3. Pleural fluid is typically unilateral or markedly asymmetric 4. Generally, empyemas form an obtuse angle with the chest wall, and due to their lenticular shape are much larger in one projection (e.g. frontal) compared to the orthogonal projection (e.g. lateral) 3. The lenticular shape (biconvex) is also suggestive of the diagnosis, as sterile transudates tend to be crescentic in shape (i.e. concave towards the lung, see empyema vs pleural effusion).
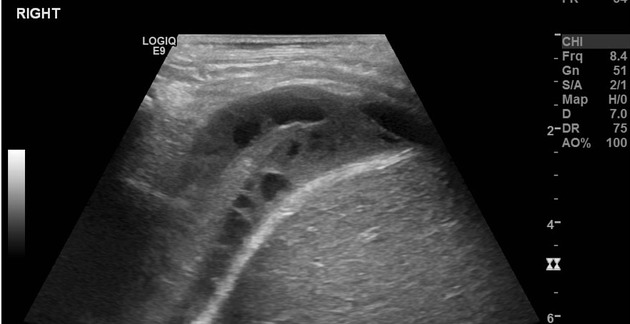
Ultrasound
The appearances of an empyema depend on the composition of the collection. Typically they are not uniformly anechoic and are often septated.
Ultrasound has a major role in enabling targeted thoracocentesis.
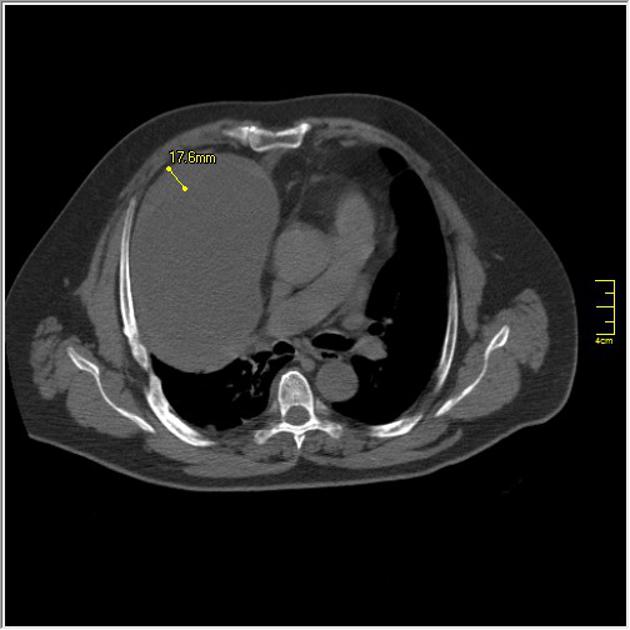
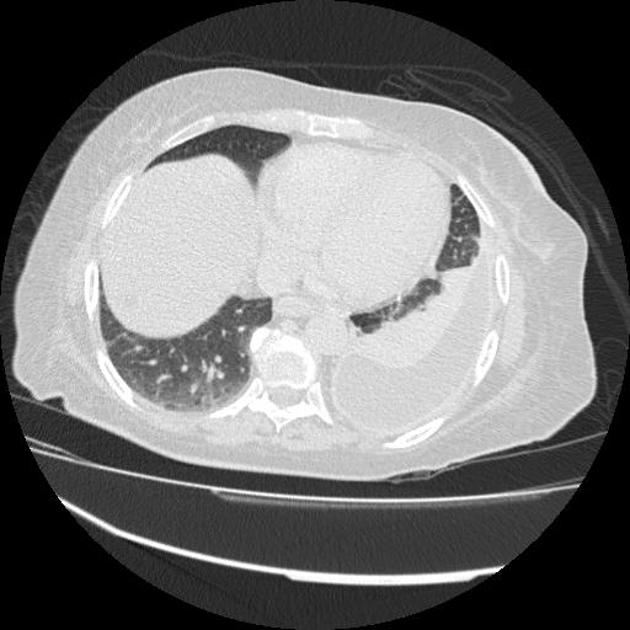
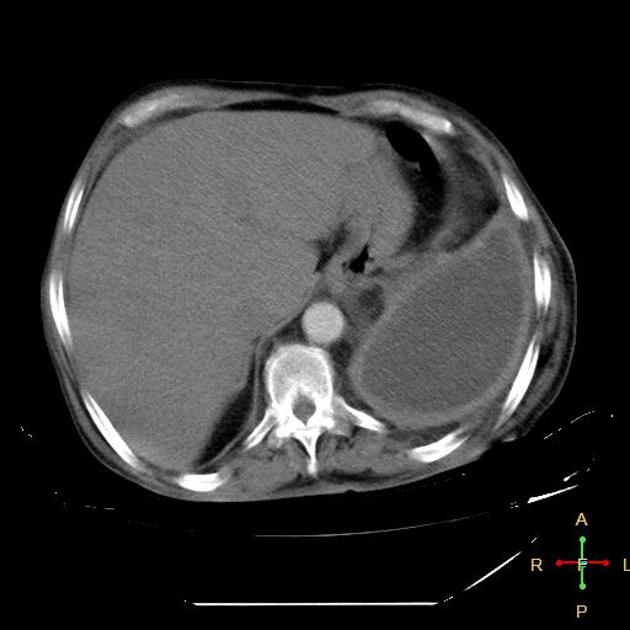
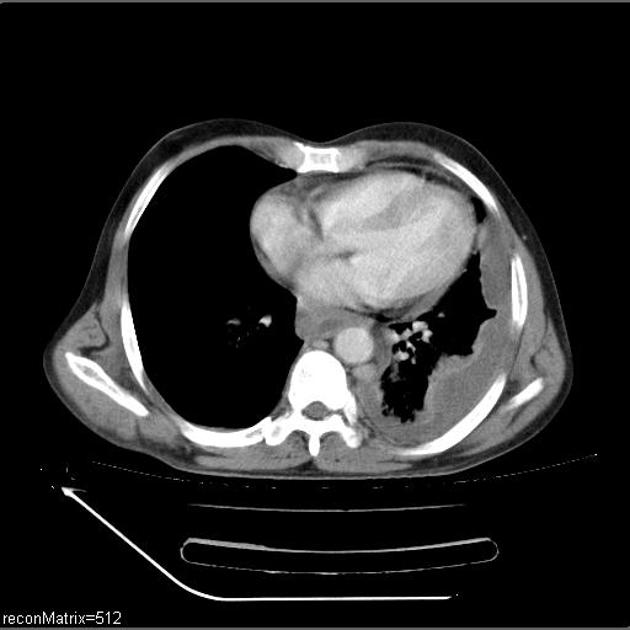
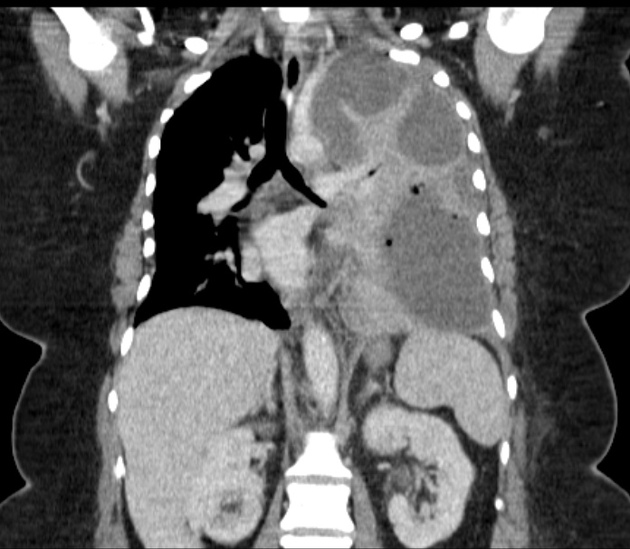
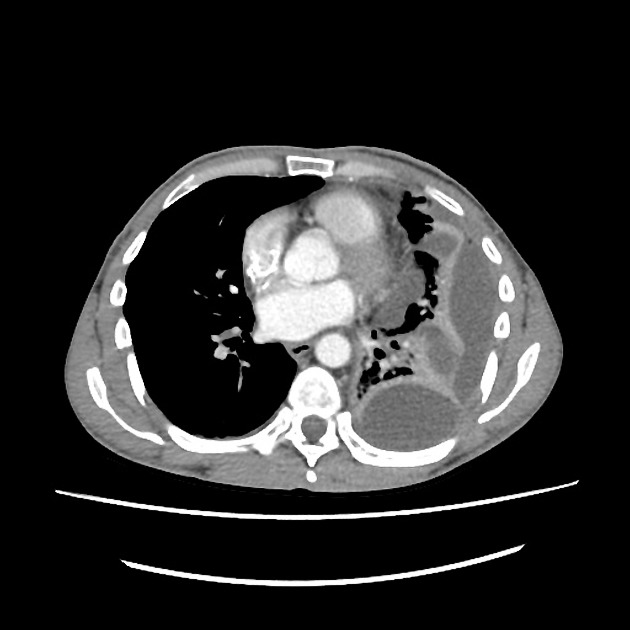
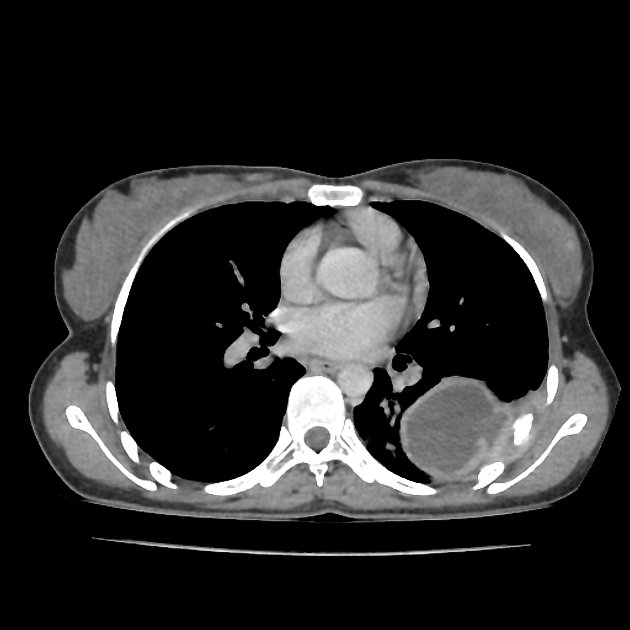
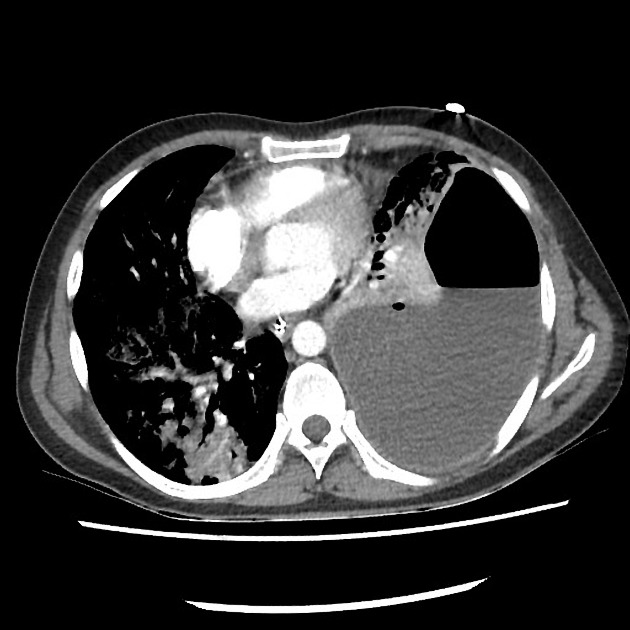
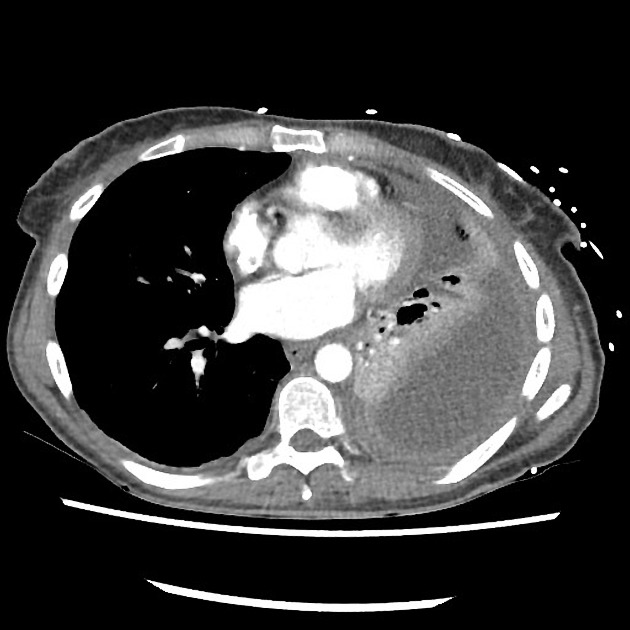
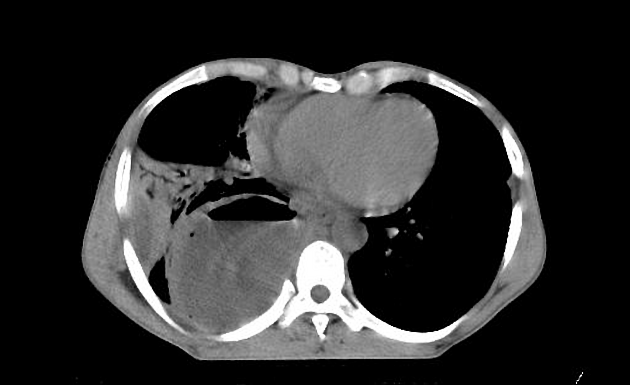
CT
Typically appears as a fluid density collection in the pleural space, sometimes with locules of gas due to gas-forming organisms or fistula. They form obtuse angles with the adjacent lung, which is displaced and compressed. The pleura is thickened due to fibrin deposition and ingrowth of vessels with enhancement which is more obvious during portal venous phase. At the margins of the empyema, the pleura can be seen dividing into parietal and visceral layers, the so-called split pleura sign, which is the most sensitive and specific sign on CT and is helpful in distinguishing an empyema from a parapneumonic effusion or a peripheral lung abscess (see: empyema vs lung abscess) 2,3. The inner walls of the empyema are smooth. There may be increased density and haziness of the extrapleural and extrathoracic fat 10. Over time, extrapleural fat hypertrophy develops external to the parietal pleura 13.
Treatment and prognosis
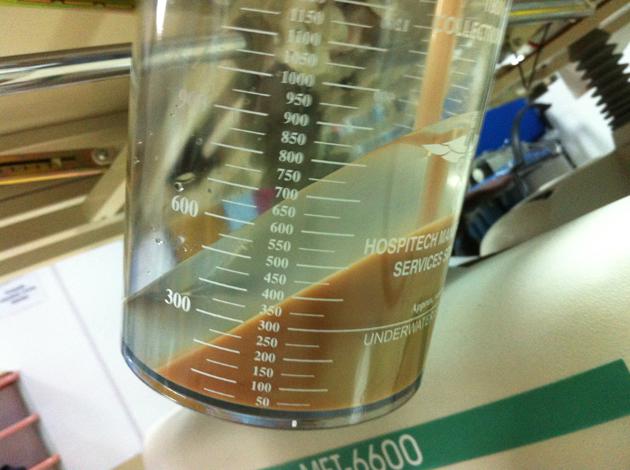
Prompt evacuation of the infected fluid along with appropriate antibiotics is the mainstay of treatment and will not only improve survival but also hopefully prevent the formation of a fibrothorax.
Evacuation may be performed with percutaneous chest tube placement often with an administration of a fibrinolytic agent (e.g. streptokinase or urokinase 8) into the pleural space to break down septations. Alternatively, video-assisted thoracic surgery (VATS), open decortication, or even Clagett thoracotomy may be performed. VATS is increasingly thought to lead to faster resolution with lower morbidity and reduced cost 5,6.
Prognosis is unsurprisingly worse in HIV/AIDS patients with reduced CD4 counts 5.
Complications
History and etymology
It may be interesting to note that the French anatomist and military surgeon, Baron Guillaume Dupuytren (1777-1835), famed for his description of Dupuytren contracture, died of a pleural empyema 6.
Differential diagnosis
General imaging differential considerations include:
-
pleural effusion from other causes, especially in the setting of inflammatory conditions
Dressler syndrome (post-myocardial infarction)
hiatus hernia (AP film)
See also
pyopneumothorax: can be thought of as a subtype of an empyema
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.