MRI protocol for rectal cancer is a group of MRI sequences put together for imaging staging of primary rectal tumors and assessment of response following neoadjuvant therapy. Modified versions of the protocol may also be used for the assessment of local recurrence.
Note: This article is intended to outline some general principles of protocol design. The specifics will vary depending on MRI hardware and software, radiologist's and referrer's preference, institutional protocols, patient factors (e.g. allergy) and time constraints.
On this page:
Preparation
Bowel preparation is not necessary for rectal MRI.
Studies are usually performed without rectal distension. Rectal distension leads to overestimation of the distance between the tumor and the anorectal junction, and errors in T staging 2.
Antispasmodic agents (e.g. hyoscine (Buscopan) or glucagon) are commonly prescribed for reducing bowel peristalsis and consequent motion artifacts 1.
Sequences
A good protocol for this purpose involves at least:
-
overviews
sagittal T2
axial T2
-
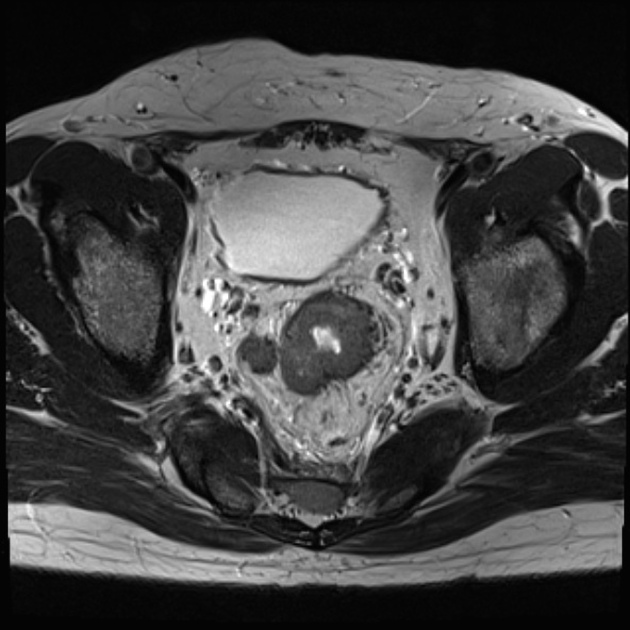
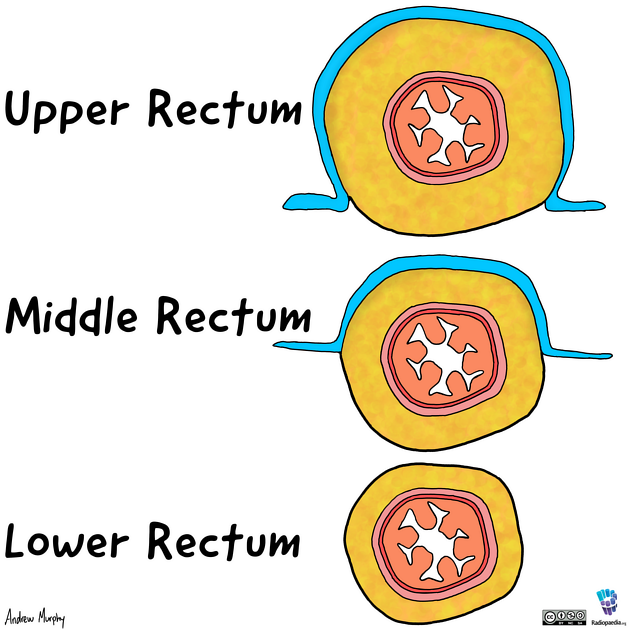
small FOV T2 through tumor
axial: perpendicular to the plane of the part of the rectum containing the tumor
coronal: parallel to the plane of the part of the rectum containing the tumor
if the tumor is long, or the part of the rectum bearing the tumor has an angulated course, multiple small field-of-view sequences may be necessary
-
optional
diffusion-weighted imaging
For restaging after chemoradiotherapy, a similar protocol may be deployed. Diffusion-weighted imaging has a greater role to play in this scenario.
Contrast enhancement is generally considered unnecessary for primary staging and restaging following chemoradiotherapy, but may be deployed for staging of local recurrences, and for the staging of locally advanced rectal cancers where the relationships to other pelvis structures such as the internal iliac vessels and sacral bone involvement are important factors in determining the surgical approach.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.