Reverse total shoulder arthroplasties (RTSA) or replacements (RTSR) are a variant of the standard total shoulder replacement (TSR). It is often the preferred method when there has been advanced damage to the rotator cuff, as it increases the range of motion by medialising the center of rotation and increasing the deltoid muscle's lever action.
On this page:
Indications
rotator cuff tear arthropathy 12
replacement after tumor surgery
complex fractures in elderly patients where the greater and lesser tuberosity fragments are involved
failed standard total shoulder replacement
Contraindications
Technique
Device structure
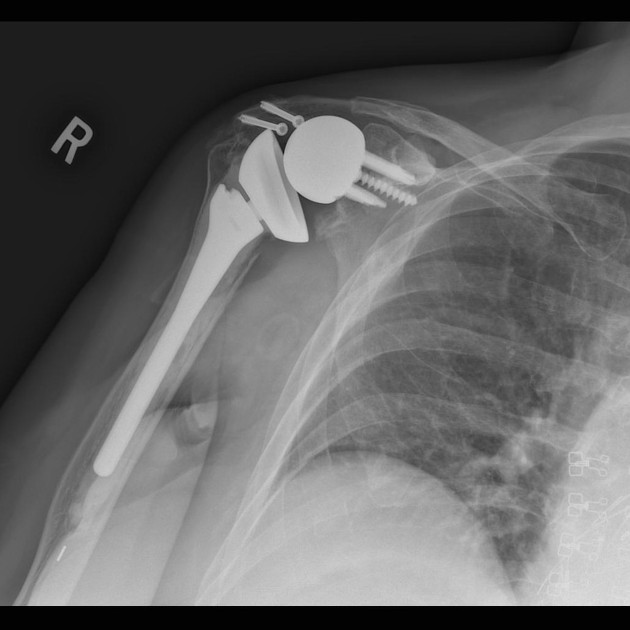
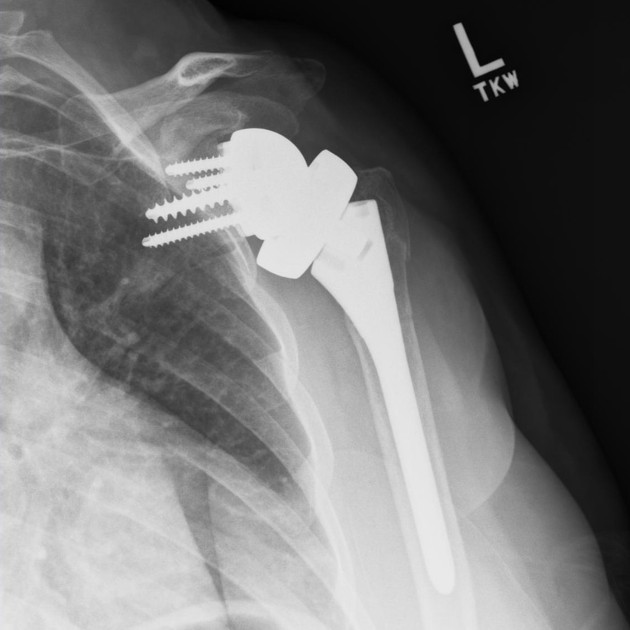
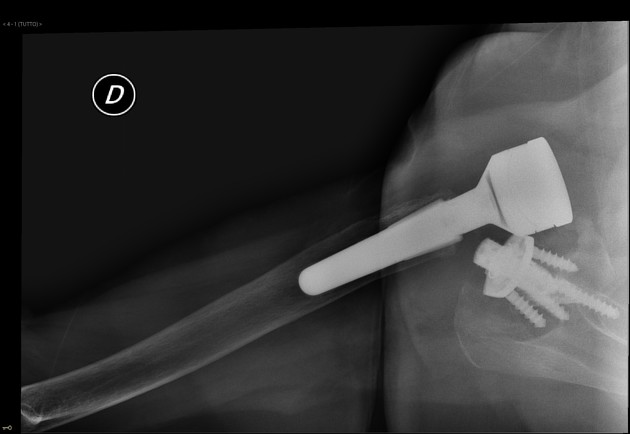
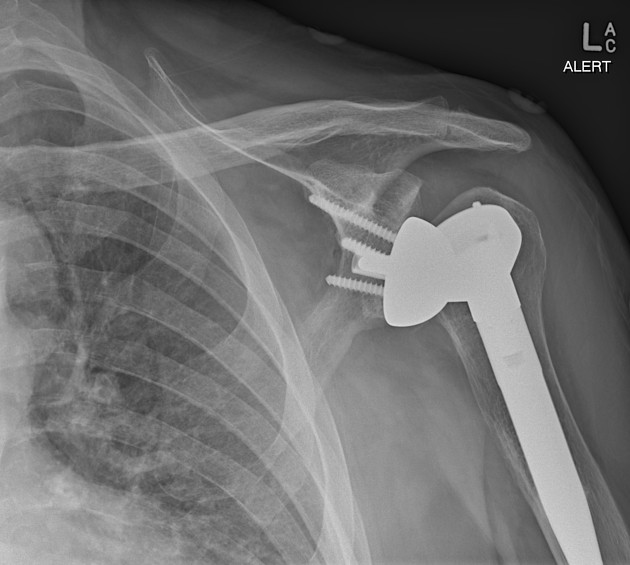
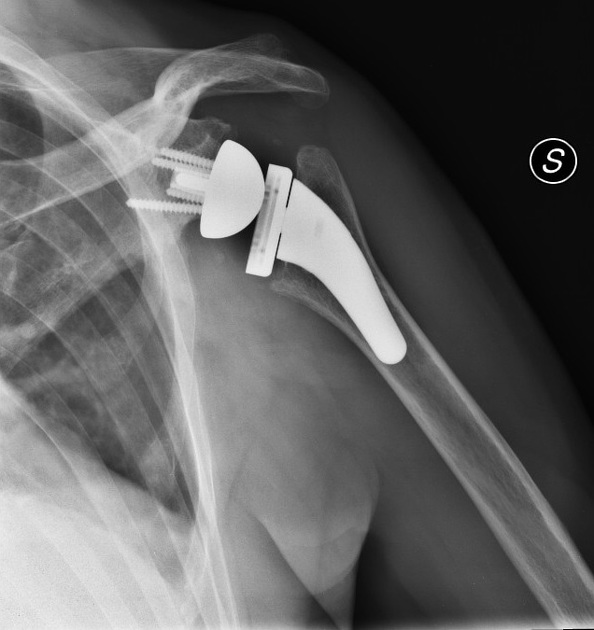
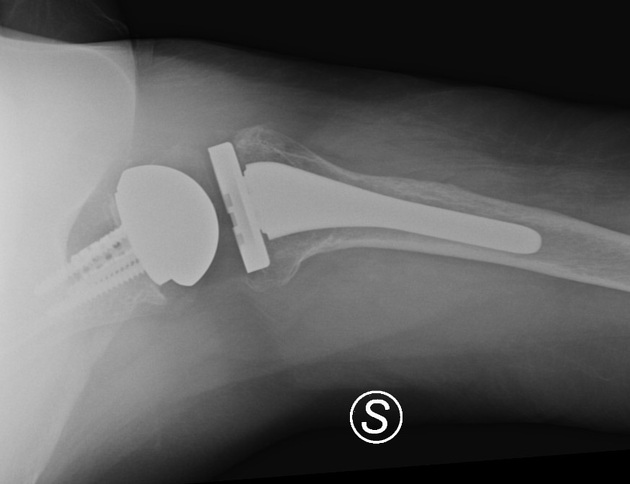
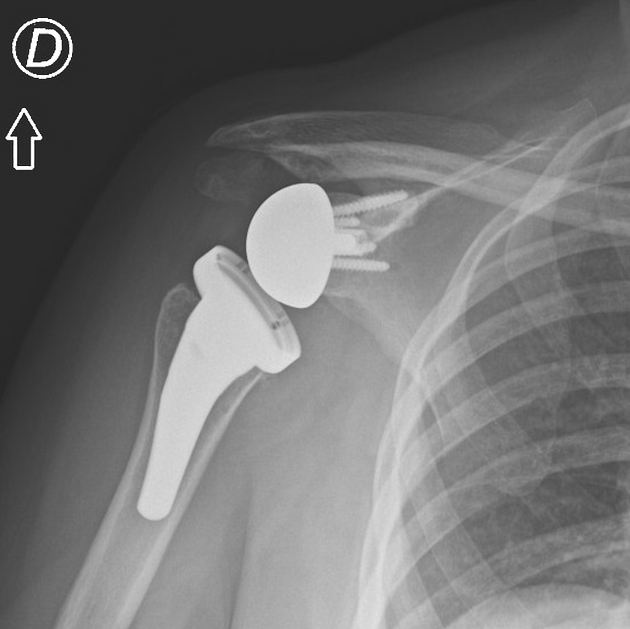
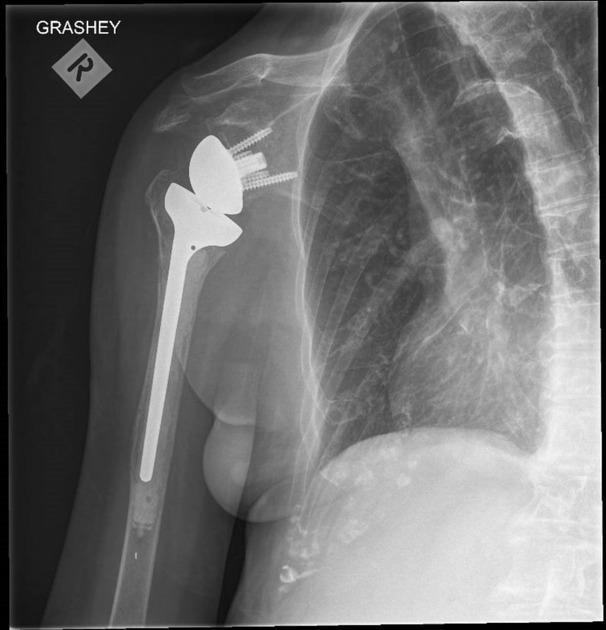
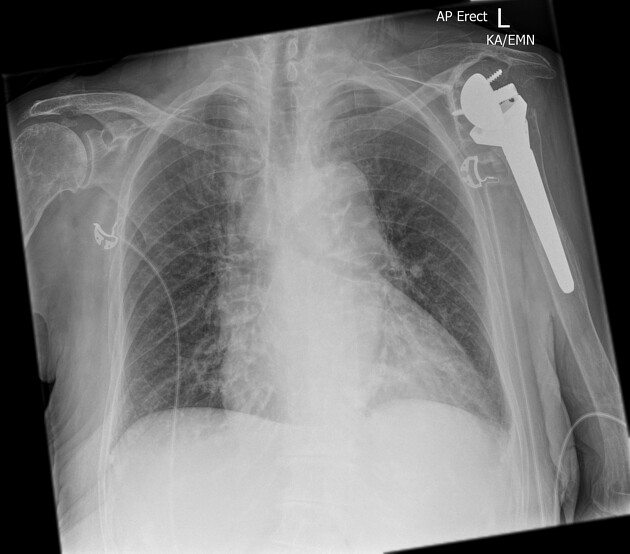
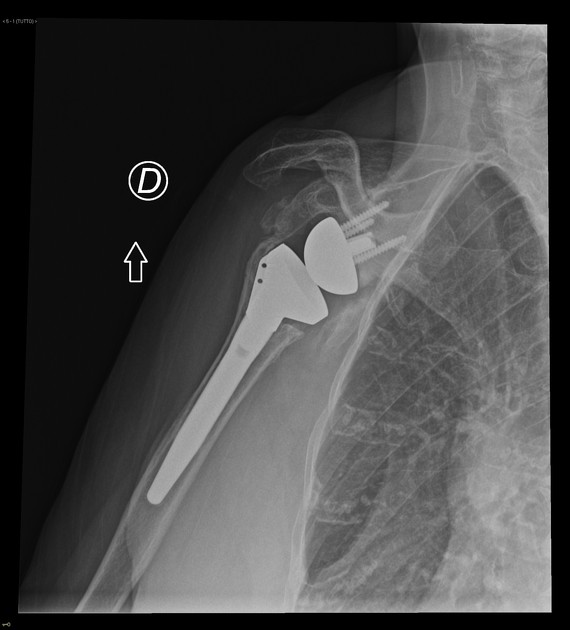
The reverse total shoulder arthroplasty flips the normal mechanical arrangement of the shoulder's ball-and-socket joint. Instead of the humeral head fitting into the glenoid, a rounded hemispheric glenoid prosthesis articulates with a socket on the humeral head prosthesis:
-
humeral components
proximal cup-shaped portion is a radiolucent polyethene insert that articulates with the glenosphere
metal stem in the proximal humeral shaft
-
glenoid components
glenosphere is the rounded metal ball of the prosthesis that attaches to a baseplate (metaglene)
baseplate (metaglene) is a specially coated metal plate that is attached to the native glenoid fossa with bicortical screws
Implant design has been classified into three types 12,13:
-
medial glenoid/medial humerus (MGMH): original Grammont prosthesis design
medialises the center of rotation to the scapula with no lateral offset of the glenosphere
2x increased risk of scapular notching 12
medial glenoid/lateral humerus (MGLH): lateral positioning of the humeral component
-
lateral glenoid/medial humerus (LGMH):
increased arc of rotation through lateral positioning of the glenoid component through thickened glenosphere, spacers, bone graft, etc
possible increased risk of baseplate failure and glenoid loosening 12
No significant difference post-operative range of motion differences, early complication rates, or revision rates have been established between the three design types with 12.
Radiographic features
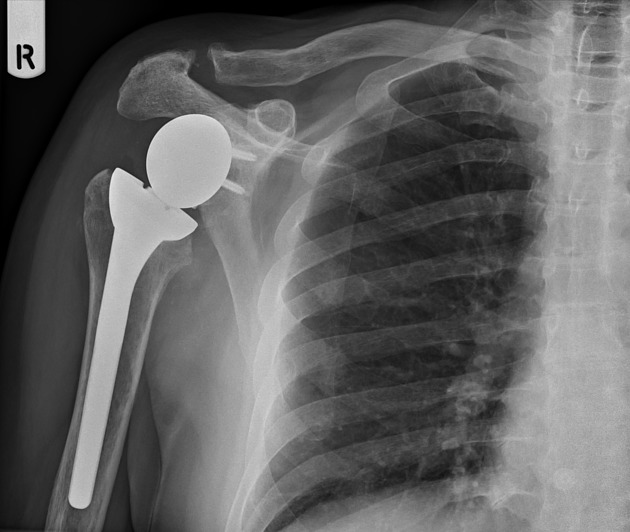
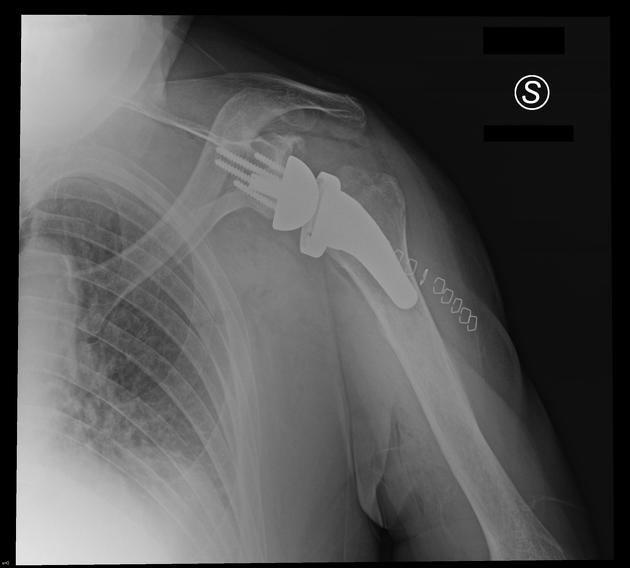
Plain radiograph
neutral AP view (Grashey view) and axillary views obtained
>2 mm of lucency around the prosthetic component is concerning for loosening
scapular notching (erosion of the inferior scapular neck) is suggestive of glenoid component failure
acromial and scapular spine fractures after reverse total shoulder arthroplasty are more common
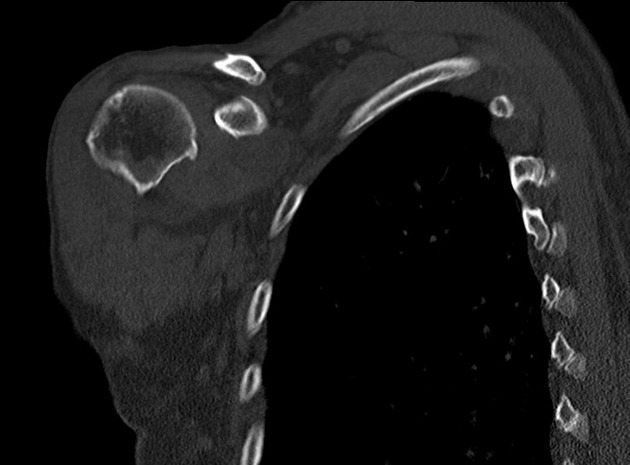
CT
better for evaluation if there is a suboptimal radiograph
as on conventional radiography, >2 mm of lucency around the prosthetic component is concerning for loosening
MRI
metal artifact reduction techniques have improved the ability to image prostheses on MRI
Ultrasound
useful for imaging the rotator cuff musculature, evaluating the prosthesis dynamically, and evaluating for joint effusion
cannot be used to evaluate for component loosening
Complications
The overall complication rate for all forms of total shoulder arthroplasty is ~15% ref. Complications for reverse TSA specifically include:
scapular notching: most common complication ~10-50% depending on prosthesis design; may not be clinically significant 12
infection: ~2.5% (range 0.7-5.2%) 12
dislocation: ~1% 12
axillary nerve injury: ~1.5% (range 0.5-2.3%) 12
-
aseptic loosening
glenoid component: most common complication affecting ~30% of all shoulder replacements 5, but decreased (~5%; range 3-10% 12) with reverse total shoulder replacements 5
humeral component: less common (~4%; range 1.2-10% 12)
-
hardware failure 12
glenosphere dissociation (rare) 14
-
periprosthetic fractures
intra-operative glenoid fracture 12
acromial/scapular spine fracture, most commonly a stress fracture 6,12
heterotopic ossification 11,12
scapular spur 12
failed bone graft incorporation 12
Outcomes
Reversing the ball and socket arrangement, the point of rotation is moved more medially, aiding the deltoid muscle which, without an intact rotator cuff, will provide most of the early abduction for the upper extremity through a level action 12. However, internal and external rotation are more limited in this arrangement.
The design is reported to have relatively good short and medium-term outcomes compared with other types of total shoulder replacements, with improved recovery time and pain scores 3. Long-term outcomes remain poorly defined.
History and etymology
French surgeon Paul-Marie Grammont (1940-2013) designs a clinically successful reverse prosthesis (where other reverse designs have failed) for arthritic shoulders with massive rotator cuff tear in 1985, in which normal anatomical prostheses could not solve the problem of restoring both joint stability and mobility 7,8.
The idea of reverse total shoulder arthroplasty thought by Grammont was an important step forward in the field of shoulder arthroplasty in fact the previous constrained prostheses (spherical or inverted spherical designs) all failed because their center of rotation remained lateral to the scapula, limiting movement and producing excessive torque at the prosthesis-bone interface of the glenoid component, thus leading to premature loosening 7,8.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.