Sialography is the imaging of the salivary glands, most commonly the parotid gland. The salivary ducts are conventionally examined fluoroscopically with high sensitivity, though cross-sectional imaging with CT or MR sialography has also been described.
On this page:
Indications
repeated pain and swelling where ultrasound does not yield any useful findings
suspected sialolithiasis or salivary duct obstruction
suspected sialectasis in chronic inflammatory disorders and autoimmune diseases (e.g. Sicca syndrome) 1
Contraindications
pregnancy
allergic to iodinated contrast media
acute sialadenitis (inflammation of salivary ducts) as this can worsen the infection 1
Types of sialography
There are three types:
conventional/fluoroscopic sialography (with or without digital subtraction)
CT sialography (ultrafast technique)
MR sialography. This uses heavily T2-weighted sequence to demonstrate the salivary ducts, thus may or may not need canalisation.
In most cases, ultrasound (with sialography, if required) is an appropriate imaging modality for the investigation of ductal pathology. In cases of sialolithiasis, ultrasound of the parotid glands is a useful, readily available, noninvasive, and inexpensive option. Ducts are best seen if dilated by obstruction.
Procedure
Technique of conventional sialography
-
control images are taken with the patient supine to assess for radiopaque calculi
lateral oblique and lateral views
using tongue depressors for submandibular
-
the patient may be asked to suck on a lemon or secretory stimulant for 2-3 minutes before sialography
to make the salivary duct opening conspicuous for cannulation
-
symptomatic parotid or submandibular duct cannulated
-
21 gauge catheter for Stensen's duct
located adjacent to the crown of the second upper molar in the buccal mucosa
gentle abduction of the cheek with thumb and index finger can help with the cannulation 1
-
24 or 27 gauge for Wharton's duct
at the base of the frenulum of the tongue
raising the tip of the tongue until it touches the hard palate can help to tense the submandibuilar duct papilla for easier cannulation
if the orifice is not visible, citric acid can be applied to promote secretion of the submandibular gland. Silver probe is then used to dilate the orifice and catheter is introduced into the duct 1
-
up to 2 mL of water-soluble contrast is instilled
care should be taken not to introduce air into the salivary ducts, as it can mimic a ductal calculus on sialography
lemon or secretory stimulant can be used to purge contrast after procedure
post procedure images are sometimes performed to assess for residual contrast
Advantages
higher spatial resolution for superior diagnostic elucidation (when the procedure is successfully achieved) with accurate delineation of second- and third-order branches
enables therapeutic approach in sialoendoscopy for removal of sialoliths, retrograde displacement of sialoliths to relieve acute obstruction, and to dilate strictures
Disadvantages
invasive procedure
the substantial failure rate of the procedure (especially submandibular sialography) is due to cannulation problems, lack of skill, lack of patient compliance, pain, etc.
radiation exposure
contrast media exposure with risk of allergic reaction
Complications
local pain
perforation of the submandibular duct
infection should be suspected if pain persists for more than 24 hours. Antibiotics should be considered if there is an infection 1.
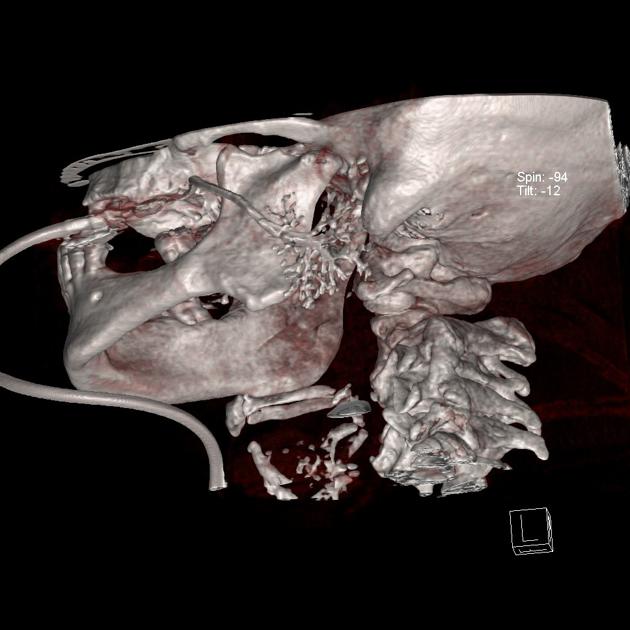
Technique of CT sialography
The procedure is essentially the same as a conventional sialogram, after which the patient is positioned in a CT in a neutral supine position. Multiplanar data acquisition allows for 3D reconstruction. Intravenous contrast material can be administered for better soft tissue evaluation, especially for parotid masses. In the 1970s and 1980s, when this technique was first introduced, slower CT scans called for delayed ductal emptying, for which atropine was given.
Advantages
assessment of glands other than the parotids is possible
better diagnosis of parenchymal pathology, excellent visualisation of the deep lobe, and better subtraction options
no special positioning required
Disadvantages
intravenous atropine is required to minimise run-off of contrast and impair ductal clearance in some cases
radiation exposure
invasive procedure
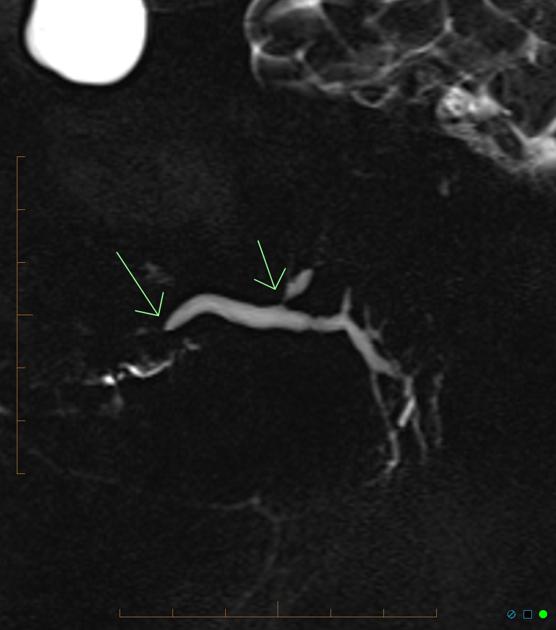
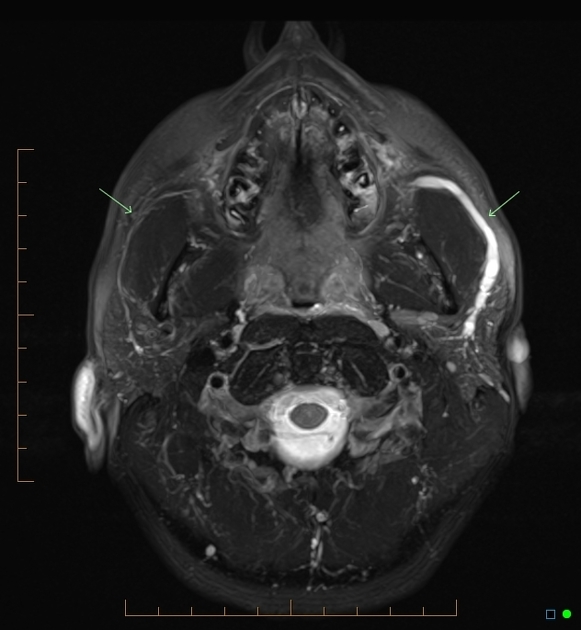
Technique of MR sialography
MRI sialography is a fairly sensitive and reliable method of evaluating the salivary glands. Fast acquisition heavily T2 weighted sequences (e.g. RARE, CISS, FISP, as used in MRCP and MR urography) brighten intraluminal fluid and display ductal morphology adequately with no need to inject contrast into the ducts. MR contrast administered intravenously is a useful adjunct.
Advantages
rapid acquisition
non-invasive
assessment of other glands possible
excellent delineation of parenchymal pathology
no special positioning required
because no cannulation is required, the risk of air bubbles simulating intraductal calculi is minimised
Disadvantages
general MRI contraindications, e.g. pacemakers, implants, claustrophobia
dental fillings, implants, bridges, etc. can cause image impairment
only first- and second-order branches can be delineated








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.