Spinal primitive neuroectodermal tumours (PNETs) are rare. Most cases are secondary to metastatic spread through the subarachnoid space from a primary intracranial tumour although rare cases of primary spinal PNETs have been reported.
This article specifically relates to spinal PNETs. For a discussion on intracranial PNETs and for a general discussion of the pathology refer to the main article: CNS primitive neuroectodermal tumour (PNET).
On this page:
Epidemiology
Unlike intracranial PNETs, those involving the spine are slightly more common in adults than in children 3. Males are more commonly affected than females.
Clinical presentation
Clinical presentation is similar to that of other intramedullary spinal tumours, with pain, weakness, and sensory changes common.
Pathology
PNETs are aggressive embryonal tumours. Histologically, they are composed of small round blue cells that are predominantly undifferentiated. There may be occasional differentiation along neuronal or glial lines 5. It has been postulated that PNETs arise from neoplastic transformation of primitive neuroepithelial cells in subependymal zones 3.
Radiographic features
Spinal PNETs may be intramedullary, extramedullary intradural or extradural in location. The most common sites of spinal involvement are the filum terminale and cauda equina (57%). Twenty-one percent occur in the cervical cord and 14% occur in the thoracolumbar area 5.
CT
May be normal 3.
CT myelography
Enlargement of the spinal cord with blockage of contrast 3.
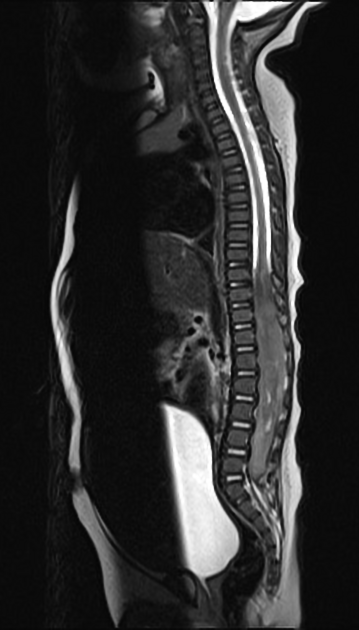
MRI
Appearance on MRI is non-specific, often mimicking other spinal lesions 6.
Reported signal characteristics include :
- T1: hypointense
- T2: hyperintense
-
T1 C+ (Gd)
- diffuse heterogeneous enhancement
- because CSF seeding commonly occurs, leptomeningeal enhancement may be seen
Treatment and prognosis
Spinal PNETs are associated with a poor prognosis (50% survival rate at 2 years) 1.
Dissemination through the CSF may produce secondary intracranial deposits. Distant metastatic spread may also occur to lungs, bone, and lymph nodes 4.
Surgery and radiotherapy are regarded as first-line management for spinal PNETs. The use of chemotherapy has been inconsistent 5.
Local recurrence is common.
Differential diagnosis
-
myxopapillary ependymoma
- the enhancement pattern is typically homogeneous (however they can have a variable enhancement pattern that, in part, depends on the amount of haemorrhage present)
- prone to haemorrhage
-
astrocytoma
- more commonly located in the thoracic and cervical regions
- ill-defined
-
metastases
- extensive peritumoural oedema
- more commonly located in the cervical and thoracic regions




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.