Subacute sclerosing panencephalitis (SSPE), also known as Dawson disease, is a rare chronic, progressive and fatal encephalitis that affects primarily children and young adults, caused by a persistent infection of immune resistant measles virus.
On this page:
Epidemiology
1 in 100,000 people infected with measles develop SSPE, with a latency of typically a decade (range 4-23 years) and thus a typical age of onset of 9-13 years of age 1,2. The marked decline of SSPE in developed nations is yet another example of the benefit of widespread vaccination.
Diagnosis
Diagnosis can be made according to the Dyken criteria, when two major and one minor criteria are present 10,12:
Major criteria
raised anti-measles antibody titres in the CSF (≥1:4) or serum (≥1:256)
-
typical or atypical clinical history:
-
typical
acute or rapidly progressive
subacute progressive
chronic progressive
chronic relapsing–remitting pattern
-
atypical
seizures
prolonged Jabbour stage I (see below)
unusual age of presentation (infancy or adulthood)
-
Minor criteria
characteristic electroencephalographic findings of periodic slow-wave (Radermecker) complexes 4-6
CSF globulin levels >20% of the total CSF protein
characteristic histopathology on brain biopsy
molecular test identification of wild-type measles virus mutated genome
Clinical presentation
Clinical presentation is gradual, progressive neuropsychological deterioration, consisting of personality change, seizures, myoclonus, ataxia, photosensitivity, ocular abnormalities, spasticity, and coma.
Jabbour et al. identified four clinical stages11:
stage I: irritability, dementia, social withdrawal, lethargy, and regression of speech
stage II: various types of movement disorders such as dyskinesia, dystonia, and myoclonus
stage III: consistent with extrapyramidal symptoms, decerebrate posturing, and spasticity
stage IV: is characterised by loss of function of cerebral cortex with signs of vegetative state, autonomic failure, and akinetic mutism
Pathology
Histopathologically, SSPE demonstrates the same changes seen in other chronic viral cerebral infections, such as HIV encephalitis and post-infectious encephalomyelitis 2.
Markers
CSF analysis may show elevated levels of:
gammaglobulin
anti-measles antibodies
Radiographic features
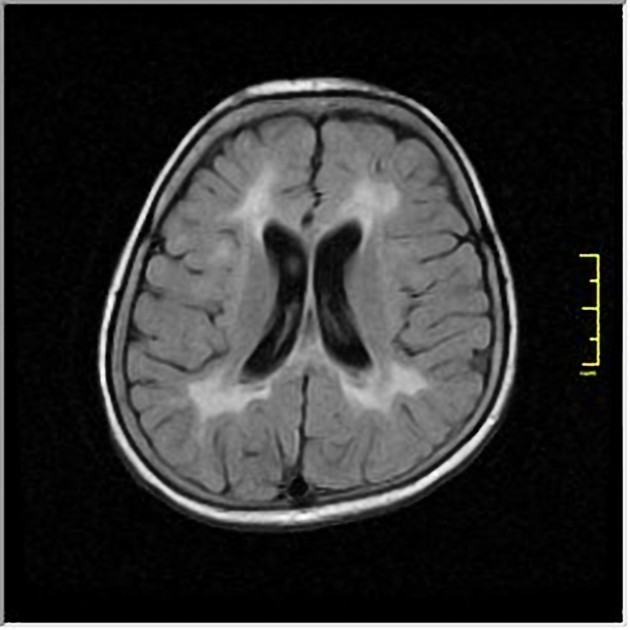
Features depend on the stage of disease.
In the acute setting, patchy asymmetric regions of white matter involvement are present, typically in the temporal and parieto-occipital lobes 9. Mild reduction in grey matter involving predominately the amygdala, frontotemporal cortex, and cingulate gyrus can also be seen in the early stage of the disease 7.
Gradually, more extensive white matter involvement develops with additional involvement of the corpus callosum and basal ganglia 1. The putamen is the most commonly involved basal ganglia, followed by globus pallidus and caudate. The thalamus is rarely involved 9. There is also variable involvement of brainstem, corona radiata and cerebellar peduncles 8 .
Eventually, a generalised encephalomalacia develops 1 and parenchymal loss may be seen in later stages. White matter hyperintensities can diminish over time in patients with clinical improvement 9.
MRI
T2/FLAIR: high signal within white matter in the parietal and temporal lobes in the acute stage 3
T1 C+ (Gd): enhancement of affected regions may occur early in the course of the disease.
-
MR spectroscopy: may demonstrate 1,3
decreased NAA: from neuronal loss
increases in choline: from demyelination
increase myo-inositol: from active gliosis
elevated lactate: from macrophagic infiltration






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.