Subdural empyema is a type of intracranial infection characterised by a suppurative collection between the dura mater and the arachnoid mater. It is commonly seen as a complication of sinusitis, otitis, mastoiditis, or surgical intervention.
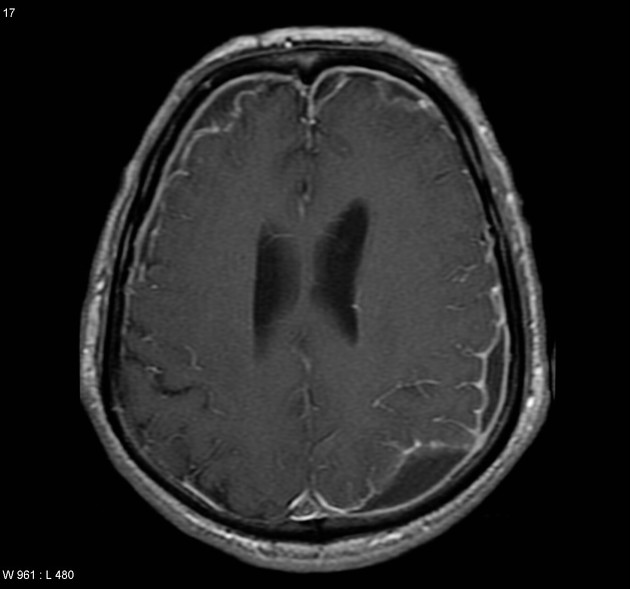
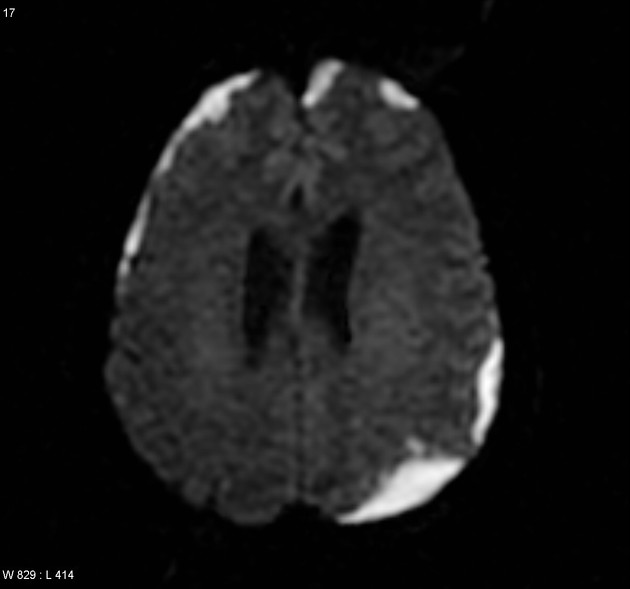
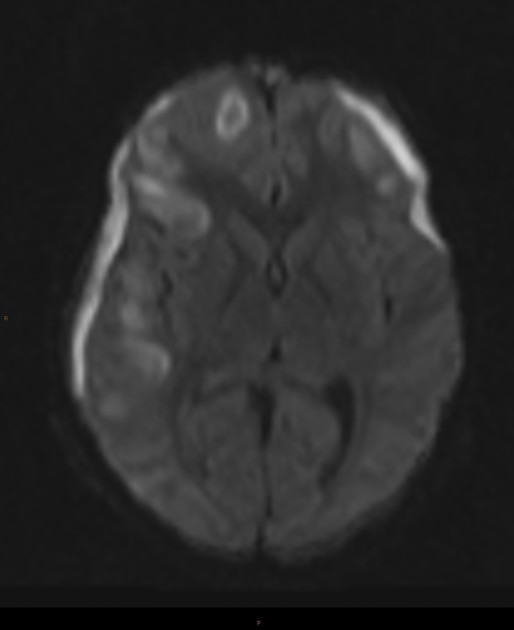
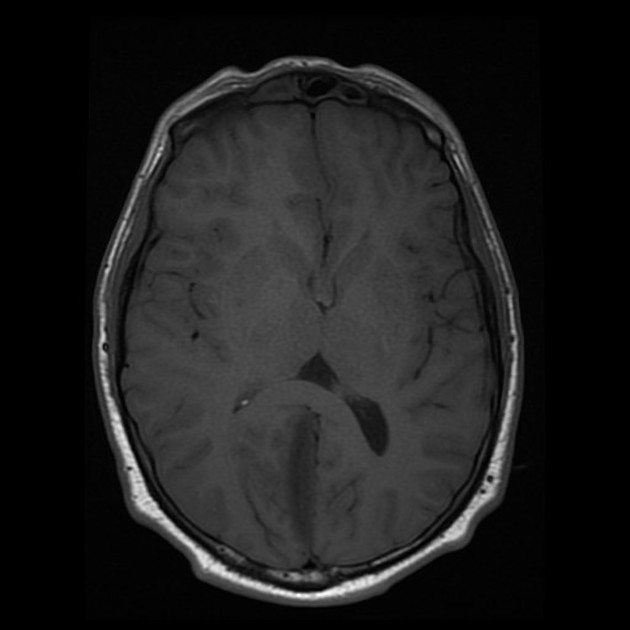
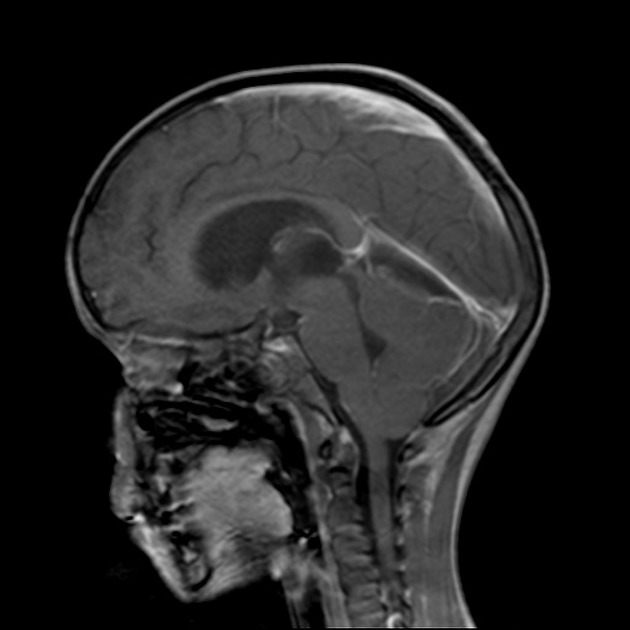
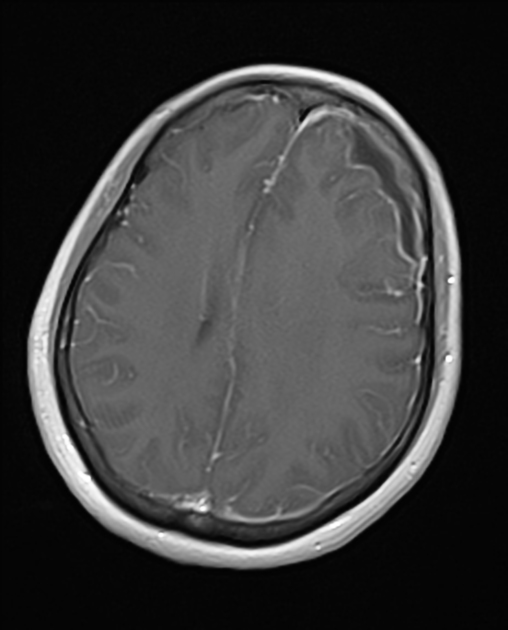
On imaging, it tends to present as a subdural collection, crescentic in shape, with marked meningeal enhancement and, on MRI, typically demonstrates restricted diffusion.
On this page:
Epidemiology
Subdural empyemas account for approximately 20-33% of all intracranial infections.
Clinical presentation
Clinical presentation depends to some degree on the aetiology. When empyemas result from sinusitis or mastoiditis they are often associated with seizures, focal neurological deficits and rapid deterioration of consciousness, progressing from obtundation to coma 1. Empyemas that occur secondary to prior trauma or surgery are usually more clinically indolent.
Pathology
In the most common scenario, patients develop subdural empyemas as a result of frontal sinusitis. There are two putative mechanisms of spread 3:
direct extension
indirect extension secondary to thrombophlebitis
Direct spread, resulting from erosion of the posterior wall of the frontal sinus (the corollary of Pott puffy tumour) is relatively uncommon. Thrombophlebitis of communicating veins is thought to be the most common cause of spread 3.
The most common causative organisms are streptococci, especially those from the Streptococcus milleri group of bacteria. Other organisms implicated in subdural empyema include Staphylococcus aureus, anaerobes and Gram-negative bacteria 4.
Aetiology
frontal sinusitis: vast majority
surgical intervention
trauma
seeding of existing subdural haematoma
Radiographic features
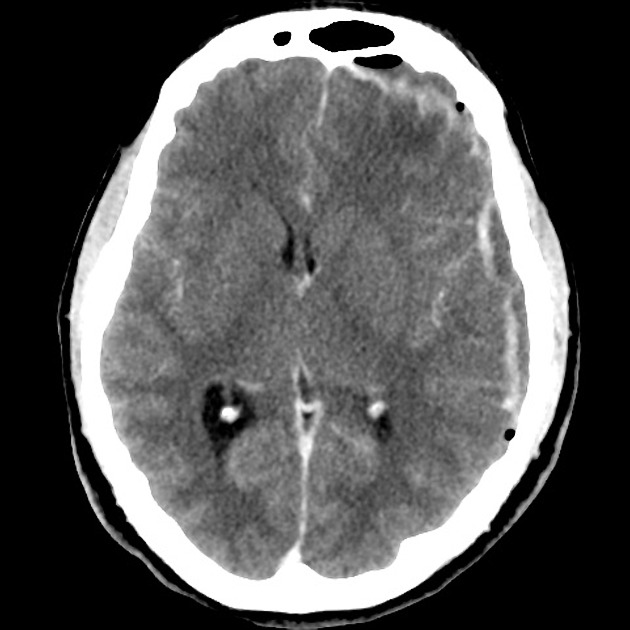
CT is usually the first investigation performed and often is the only one required, as patients usually expediently proceed to the surgical theatre for evacuation.
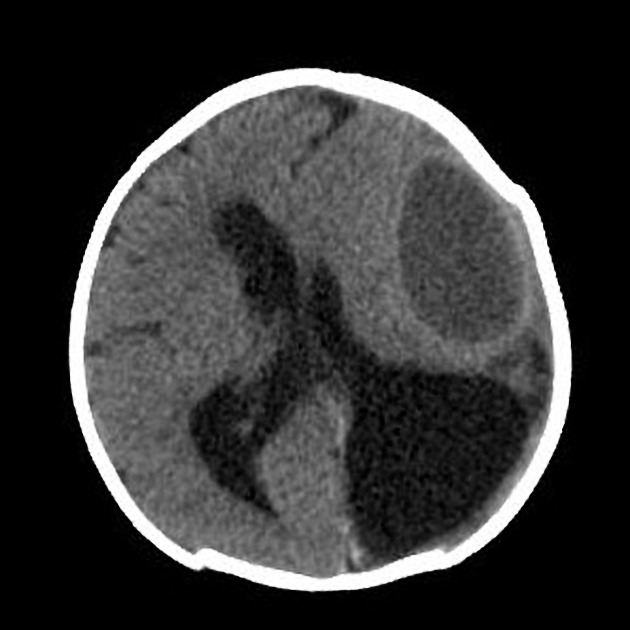
CT
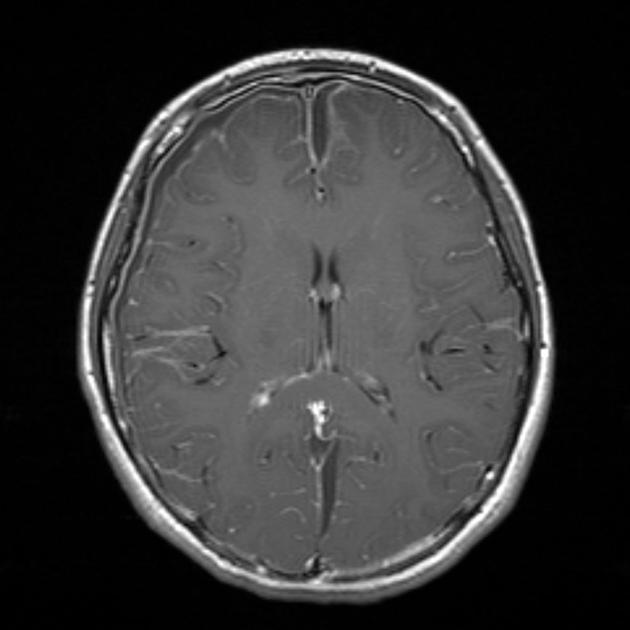
Subdural empyemas typically resemble subdural haematomas in their shape and relationship to sutures and dural reflections. They are typically crescentic in shape (compared to epidural empyemas which are typically lentiform), although collection pockets may appear biconvex. A surrounding membrane that enhances intensely and uniformly following contrast administration is typical.
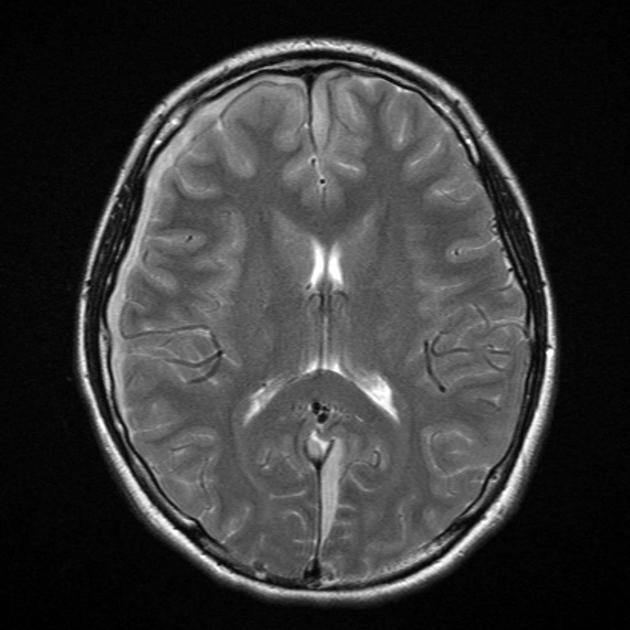
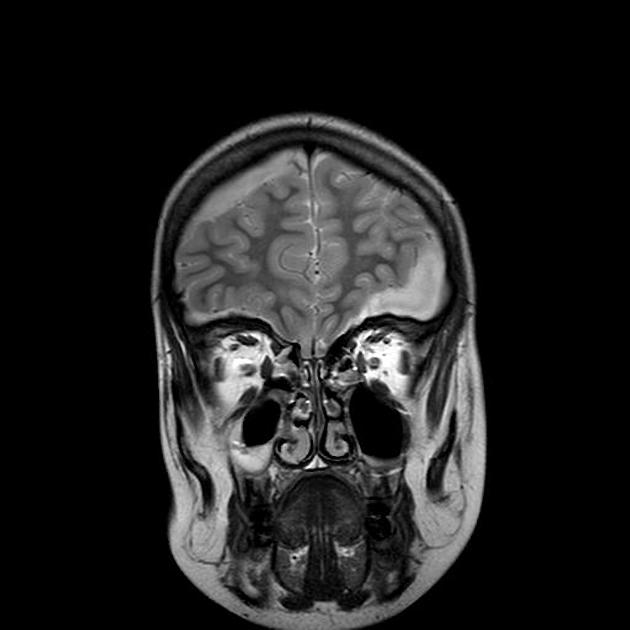
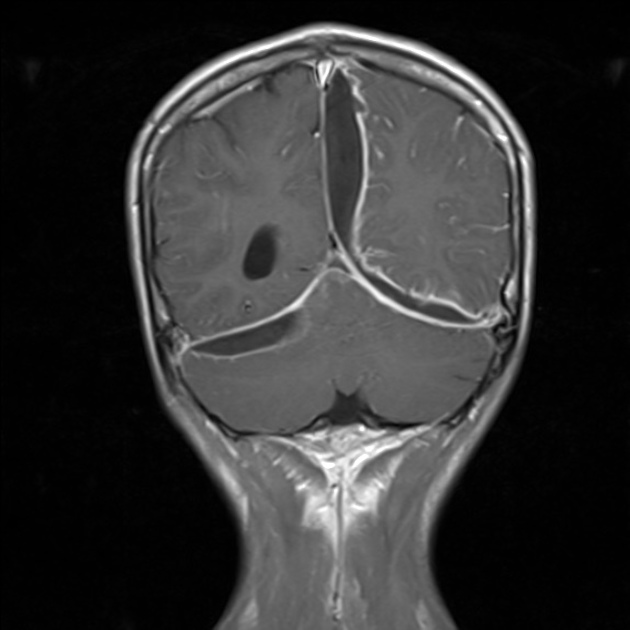
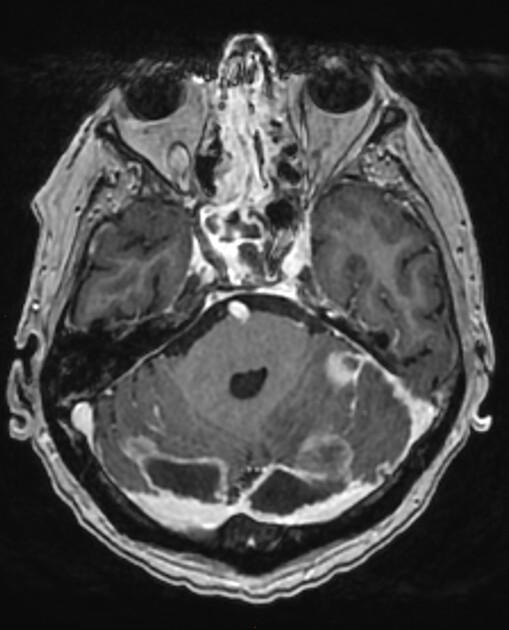
MRI
Appearance on MRI is similar to that on CT, although contrast enhancement is more readily detected. Furthermore, the content of the collection will typically demonstrate restricted diffusion.
MRI is also more sensitive to the complications of subdural empyemas, e.g. cerebritis, cerebral abscess, and venous thrombosis.
Treatment and prognosis
Successful treatment is predicated on prompt diagnosis, followed by surgical evacuation of the collection and administration of appropriate antibiotics.
Mortality associated with subdural empyemas approaches 10%, compared with approximately 15-40% in the pre-CT era 1.
Complications
Complications are relatively common and may be the cause of presentation. They include:
cortical vein thrombosis with or without venous infarction
cerebritis or cerebral abscess formation






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.