Todd paralysis, also known as Todd paresis or postictal paralysis, describes transient focal neurological deficits after an epileptic seizure. It is an important clinical and imaging differential diagnosis of ischaemic stroke presenting with a seizure.
On this page:
Epidemiology
The incidence of Todd paralysis, in one study of patients with seizures confirmed with video-electroencephalography monitoring, was found to be 13.4% 1. In comparison, seizure after stroke, the primary differential diagnosis for this phenomenon, occurs in 8.6% of strokes, with only 3.4% occurring within the first 24 hours of stroke onset 2.
Clinical presentation
Todd paralysis is a heterogeneous clinical syndrome, encompassing a variety of unilateral focal neurological deficits that occur on the side of the body contralateral to the seizure focus 1-3, such as:
paresis 1-3
aphasia 1-3
gaze palsy 1-3
sensory disturbances (e.g. neglect, anaesthesia) 1-3
These clinical features manifest immediately after the seizure, and most episodes of Todd paralysis are brief, with one study finding that the clinical features lasted a median of approximately three minutes 1-3. The duration may be longer in patients with tonic-clonic generalised seizures, compared to those with focal seizures 1-3.
This is in contrast with seizures after stroke which demonstrate focal neurological defects of a prolonged duration, depending on the severity of the stroke 1-3. Indeed, in patients with Todd paralysis, continued focal neurological deficits beyond more than a few minutes usually indicates the presence of a focal brain lesion as the underlying seizure aetiology, or persisting non-convulsive seizures 4.
Pathology
The exact pathophysiology of Todd paralysis remains uncertain 1-4. The leading hypotheses consider either cortical neuronal exhaustion from hypoxia or substrate depletion causing increased inhibition, particularly of the primary motor cortex 1-4. However, there are numerous other theories, including the presence of a temporary vascular steal phenomenon, effects of an underlying vascular disease, and release of endogenous inhibitory substances 1-4. It is likely that the aetiology is multifactorial in nature 1-4.
This pathophysiology is thought to be similar to that underlying hemiconvulsion-hemiplegia epilepsy syndrome 4.
Radiographic features
CT
Non-contrast CT brain is generally unremarkable unless there is an underlying condition 2,5-7.
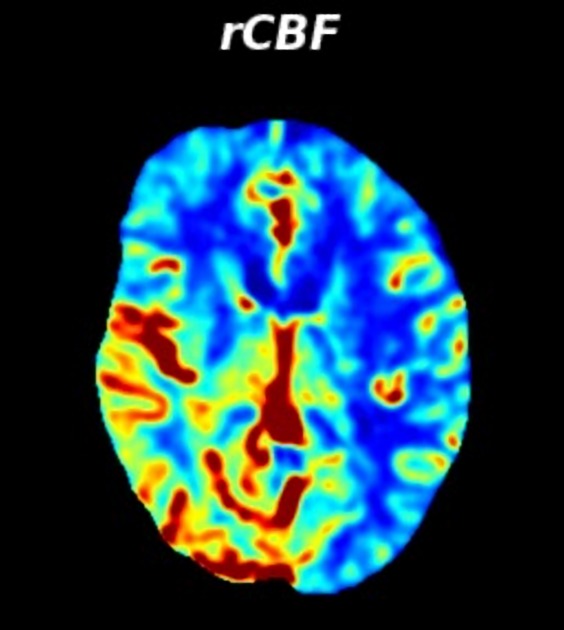
CT perfusion
CT perfusion anomalies are often noted in patients with Todd paralysis, however, findings across studies are not consistent. Many studies describe transient hyperperfusion in the cerebral hemisphere ipsilateral to that of the seizure focus (and therefore contralateral to the focal neurological defect) as demonstrated by electroencephalography, however other studies describe transient hypoperfusion in the same region 5-7. The region of abnormality typically does not correspond to a single vascular territory.
The region of perfusion anomaly is also variable in morphology and may have a cortical ribbon pattern, be multi-lobar in appearance, or may involve the whole hemisphere 5-7. These anomalies normalise once symptoms have resolved 5-7. The variability of CT perfusion findings supports the notion that the aetiology of Todd paralysis is likely to be multifactorial, and that perfusion status is simply just one of many factors at play in this phenomenon.
An important imaging differential diagnosis of this appearance is that of luxury perfusion.
CT angiography
CT angiography is importantly unremarkable with no demonstrable large vessel occlusion, providing a key distinction between this phenomenon and ischaemic stroke 2,5-7.
MRI
Brain MRI may demonstrate features consistent with a seizure, most commonly transient increased T2 signal, best appreciated on FLAIR, at the epileptic focus 10. This may be associated with transient DWI and ADC changes, and variable transient post-contrast T1 signal changes 10.
Treatment and prognosis
No specific treatment is necessary for patients with confirmed Todd paralysis other than general seizure management 1-4. Importantly, in cases where ischaemic stroke has not yet been excluded as the diagnosis, use of thrombolytic agents such as alteplase is relatively contraindicated if a seizure has occurred 9.
History and etymology
The condition is eponymously named after Robert Bentley Todd (1809-1860), a British neurologist, who described the phenomenon in 1849 10,11. However, the first description was actually made by Louis François Bravais (1801-1843), a French neurologist, who described it in less detail in 1827 10,12.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.