Transverse myelitis, also known as acute transverse myelitis, is an inflammatory condition affecting both halves (ventral and dorsal) of the spinal cord and associated with rapidly progressive motor, sensory, and autonomic dysfunction.
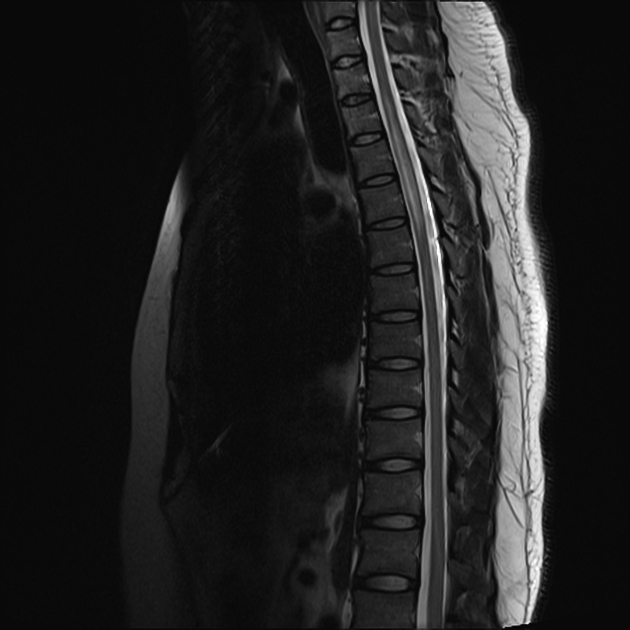
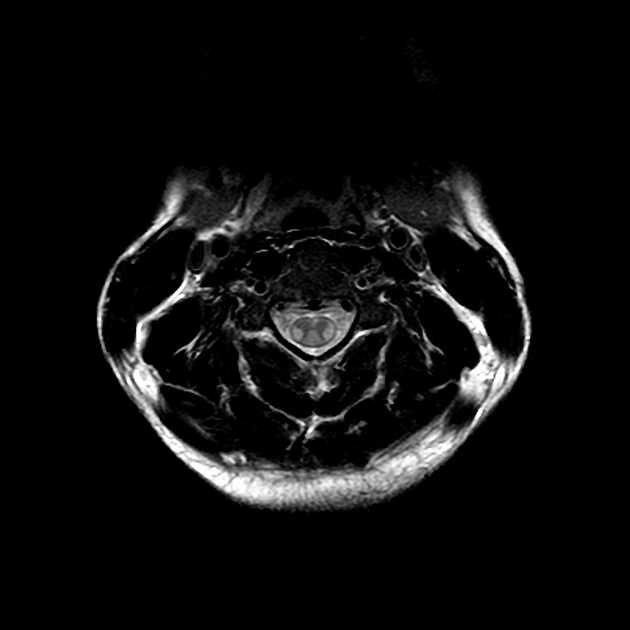
MRI is the most useful imaging modality, which generally shows a long segment (3-4 segments or more) of T2 increased signal occupying greater than two-thirds of the cross-sectional area of the cord, with variable pattern of enhancement and no diffusion restriction.
On this page:
Epidemiology
The incidence of acute transverse myelitis is 1-4 cases per million people per year 7. It affects individuals of all ages with peaks at ages 10-19 years and 30-39 years 7. There is no sex or familial predisposition and usually no prior history of neurologic abnormality.
Clinical presentation
The clinical course is highly variable but typically evolves over hours or days.
Symptoms and signs are typically bilateral and include:
para- or tetraparesis
sensory impairment with sensory level
sphincter dysfunction
Diagnosis
As the diagnosis does not have a sensitive and specific laboratory test, histology is usually not obtained, particularly as biopsy of the spinal cord has a high morbidity. Imaging features overlap with other inflammatory and neoplastic entities. A set of diagnostic criteria have been proposed by the Transverse Myelitis Consortium Working Group 7:
-
inclusion criteria
development of sensory, motor, or autonomic dysfunction attributable to the spinal cord
bilateral signs and symptoms (though not necessarily symmetric)
clearly defined sensory level
exclusion of extra-axial compression by neuroimaging (MRI or myelography; CT is not adequate)
inflammation within the spinal cord demonstrated by CSF pleocytosis or increased IgG index or gadolinium enhancement
progression to nadir between 4 hours and 21 days after the onset of symptoms
-
exclusion criteria
radiation to the spine within the last 10 years
arterial distribution clinical deficit consistent with thrombosis of the anterior spinal artery
abnormal flow voids on the surface of the spinal cord consistent with spinal dural arteriovenous fistula
-
exclusion criteria for idiopathic acute transverse myelitis
connective tissue disease
CNS infection
brain MRI abnormalities suggestive of multiple sclerosis
history of clinically apparent optic neuritis
Pathology
Pathology may reveal perivascular lymphocytic infiltrates, necrosis, and demyelination.
Etiology
In many cases, it is idiopathic, i.e. no underlying cause is identified.
In some patients, however, an etiology is identified 11:
acute infection (most commonly viral)
post-infection, parainfectious, or post-vaccination (e.g. ADEM)
myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD)
connective tissue disease (e.g. systemic lupus erythematosus, rheumatoid arthritis, Sjögren disease, antiphospholipid syndrome)
systemic malignancy (e.g. paraneoplastic)
atopy and allergy (atopic myelitis) 9
Radiographic features
Lesions may occur anywhere within the cord, with the thoracic cord being the most frequently involved site.
CT
variable enlargement of the spinal cord
variable contrast enhancement patterns (including no enhancement)
MRI
Up to 40% of cases have no findings on MRI 8. In the remainder, the appearance is variable and non-specific:
there is a large variation in lesion size, however, they most commonly extend for 3-4 spinal segments (i.e. longitudinally extensive transverse myelitis) 3
lesions typically occupy greater than two-thirds of the cross-sectional area of the cord 3
there is variable enlargement of the spinal cord
Typical signal characteristics include:
T1: isointense or hypointense
T2: poorly delineated hyperintense signal
T1 C+ (Gd): variable enhancement patterns (none, diffuse, patchy, peripheral)
Treatment and prognosis
Treatment of secondary acute transverse myelitis depends on the underlying cause. Corticosteroids and other immunosuppressives are typically given empirically in idiopathic cases.
One-third of patients recover with little or no sequelae, one-third are left with a moderate degree of permanent disability, and one-third are left with severe disabilities 3.
Differential diagnosis
General imaging differential considerations include:
-
spinal cord is usually enlarged
hyperintense on T2 weighted images and DWI
post-contrast enhancement may or may not be present (enhancement is usually present in the subacute stage)
signal intensity abnormality may be limited to the central grey matter or may involve most of the cross-sectional area of the cord
signal abnormality typically extends over multiple vertebral body segments
can occur at any location in the cord but has a propensity for the upper thoracic or thoracolumbar regions
vertebral body T2 hyperintensity may occasionally be seen (due to concomitant infarction)
-
invariable spinal cord expansion
the majority show at least some contrast enhancement
commonly associated with cysts and syringohydromyelia
may have evidence of prior hemorrhage
slowly progressive clinical course













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.