Vasa praevia
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
View Yuranga Weerakkody's current disclosuresAt the time the article was last revised Arlene Campos had no financial relationships to ineligible companies to disclose.
View Arlene Campos's current disclosures- Vasa previa
Vasa praevia refers to a situation where there are aberrant fetal vessels crossing over or in close proximity to the internal cervical os, ahead of the fetal presenting part. These vessels are within the amniotic membranes, without the support of the placenta. Vasa praevia is a rare but potentially catastrophic cause of antepartum haemorrhage.
On this page:
Epidemiology
Vasa praevia occurs in 0.6 per 1000 pregnancies 11.
Risk factors
IVF pregnancy
Clinical presentation
Prior to rupture of the amniotic membrane during labour, compression of the vulnerable fetal blood vessels by the presenting part may lead to fetal heart decelerations and bradycardia.
However once ruptured, vasa praevia will result in brisk vaginal bleeding with rapid fetal exsanguination.
Pathology
Vasa praevia can be of two types:
type I (~90% 3): abnormal fetal vessels connect a velamentous cord insertion with the main body of the placenta
-
type II
abnormal vessels connect portions of a bilobed placenta
placenta with a succenturiate lobe: due to this association, vasa praevia needs to be excluded in patients with variant placental morphology
These vessels are unsupported by Wharton jelly or placental tissue and are at risk of rupture during labour.
Radiographic features
Ultrasound
Sonographic features are considered generally specific (~90%) 2.
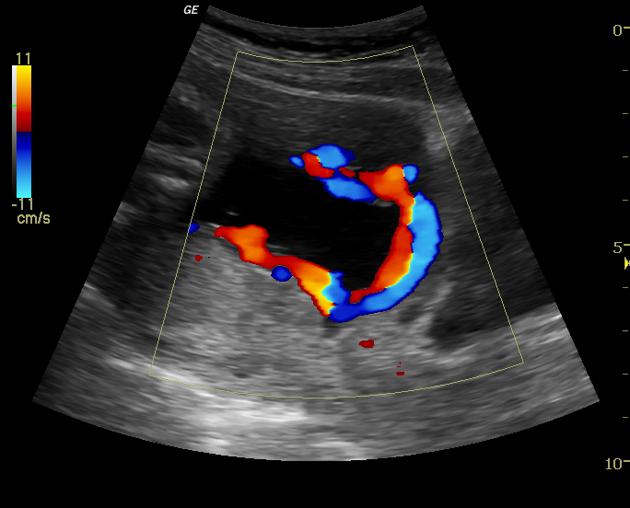
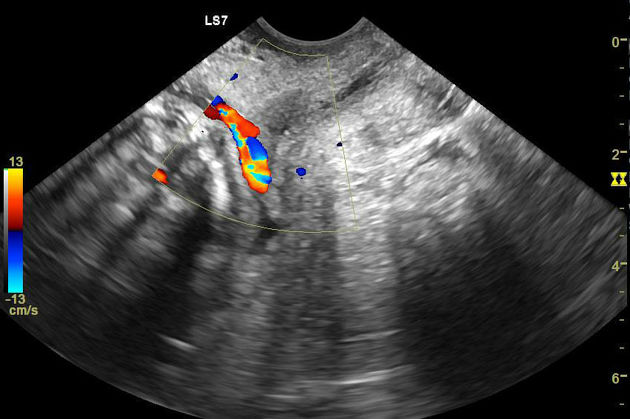
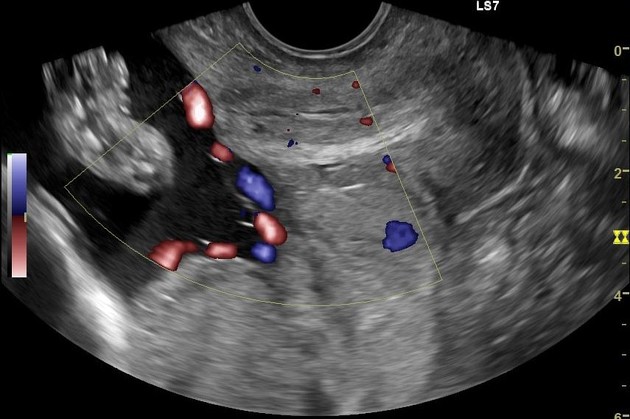
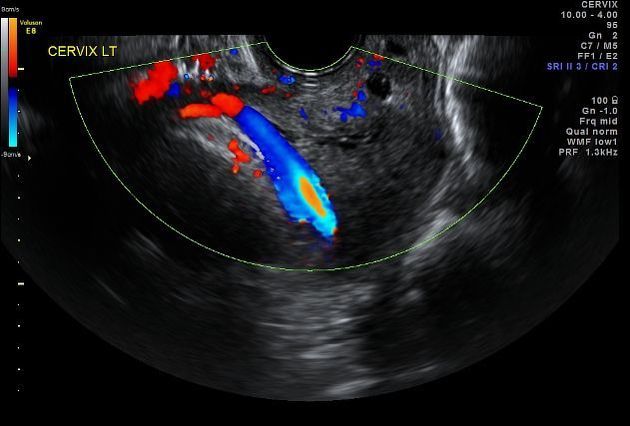
The diagnosis is often made with transabdominal colour Doppler sonography demonstrating flow within vessels that are seen overlying the internal cervical os. Greyscale images may suggest the diagnosis if there are echogenic parallel or circular lines within the placenta near the cervix.
Occasionally a transvaginal scan is required to better visualise aberrant vessels. Transvaginal ultrasound has a reported sensitivity of 100% and specificity of 99-99.8% when performed with colour Doppler 12.
Treatment and prognosis
If recognised antenatally, vasa praevia usually requires an elective caesarean section to avoid the risk of complications during vaginal delivery.
If recognised intrapartum, an emergency caesarean section is usually performed.
Differential diagnosis
On antenatal ultrasound consider:
marginal placenta praevia: where prominent maternal vessels are appreciated at the edge of the placenta
References
- 1. Fadl S, Moshiri M, Fligner CL, Katz DS, Dighe M. Placental Imaging: Normal Appearance with Review of Pathologic Findings. Radiographics : a review publication of the Radiological Society of North America, Inc. 37 (3): 979-998. doi:10.1148/rg.2017160155 - Pubmed
- 2. Catanzarite V, Maida C, Thomas W et-al. Prenatal sonographic diagnosis of vasa previa: ultrasound findings and obstetric outcome in ten cases. Ultrasound Obstet Gynecol. 2001;18 (2): 109-15. doi:10.1046/j.1469-0705.2001.00448.x - Pubmed citation
- 3. Hasegawa J, Farina A, Nakamura M et-al. Analysis of the ultrasonographic findings predictive of vasa previa. Prenat. Diagn. 2010;30 (12-13): 1121-5. doi:10.1002/pd.2618 - Pubmed citation
- 4. Lee W, Lee VL, Kirk JS et-al. Vasa previa: prenatal diagnosis, natural evolution, and clinical outcome. Obstet Gynecol. 2000;95 (4): 572-6. - Pubmed citation
- 5. Hertzberg BS, Kliewer MA. Vasa previa: prenatal diagnosis by transperineal sonography with Doppler evaluation. J Clin Ultrasound. 1998;26 (8): 405-8. J Clin Ultrasound (link) - Pubmed citation
- 6. Nimmo M, Kinsella D, Andrews H. MRI in Pregnancy: The Diagnosis of Vasa Previa by Magnetic Resonance Imaging. Bristol Med Chir J. 1988;103(2):12. PMC5113616 - Pubmed
- 7. Oyelese Y, Jha RC, Moxley MD et-al. Magnetic resonance imaging of vasa praevia. BJOG. 2003;110 (12): 1127-8. BJOG (link) - Pubmed citation
- 8. Gagnon R, Morin L, Bly S et-al. Guidelines for the management of vasa previa. J Obstet Gynaecol Can. 2009;31 (8): 748-60. - Pubmed citation
- 9. Edward I. Bluth. Ultrasound. (2000) ISBN: 9780865778610 - Google Books
- 12. Ruiter L, Kok N, Limpens J et al. Incidence of and Risk Indicators for Vasa Praevia: A Systematic Review. BJOG. 2016;123(8):1278-87. doi:10.1111/1471-0528.13829 - Pubmed
- 12. Ruiter L, Kok N, Limpens J et al. Systematic Review of Accuracy of Ultrasound in the Diagnosis of Vasa Previa. Ultrasound Obstet Gynecol. 2015;45(5):516-22. doi:10.1002/uog.14752 - Pubmed
- Carol B. Benson, Edward I. Bluth. Ultrasonography in Obstetrics and Gynecology. (2008) ISBN: 9781588906120 - Google Books
Incoming Links
Related articles: Pathology: Genitourinary
- obstetrics
-
first trimester
- ultrasound findings in early pregnancy
- embryo/fetus
- beta-hCG levels
- confirming intrauterine gestation
- pregnancy of unknown location (PUL)
- first trimester vaginal bleeding
- early structural scan
- aneuploidy testing
-
second trimester
- fetal biometry
- amniotic fluid volume
- fetal morphology assessment
- soft markers
- amnioreduction
- Doppler ultrasound
- nuchal translucency
- 11-13 weeks antenatal scan
- chorionic villus sampling (CVS) and amniocentesis
- other
- placenta
- placental anatomy
- placental developmental abnormalities
- placenta praevia
- spectrum of abnormal placental villous adherence
- abnormalities of cord insertion
- abruptio placentae
- placental pathology
- vascular pathologies of placenta
- placental infections
- placental masses
- molar pregnancy
- twin placenta
- miscellaneous
-
first trimester
- gynaecology
- acute pelvic pain
- chronic pelvic pain
- uterus
- ovaries
- ovarian follicle
- ovarian torsion
- pelvic inflammatory disease
- ovarian cysts and masses
- paraovarian cyst
- polycystic ovaries
- ovarian hyperstimulation syndrome
- post-hysterectomy ovary
- cervix
- fallopian tube
- other
- male genital tract
- prostate gland
- transrectal ultrasound
- prostate tumours
- infections of the prostate
-
prostatitis
- acute bacterial prostatitis
-
chronic prostatitis
- chronic bacterial prostatitis
- chronic prostatitis and chronic pelvic pain syndrome (CPPS)
- asymptomatic inflammatory prostatitis
- granulomatous prostatitis
- emphysematous prostatitis
- prostatic abscess
-
prostatitis
- benign prostatic hypertrophy
- cystic lesions of the prostate
- prostatic calcification
- prostatic infarction
- testes
-
unilateral testicular lesion
- testicular torsion
- orchitis
- testicular trauma
-
germ cell tumours of the testis
- testicular seminoma
-
non seminomatous germ cell tumours
- mixed germ cell tumour
- yolk sac tumour (endodermal sinus tumour)
- embryonal cell carcinoma
- choriocarcinoma
- testicular teratoma
- testicular epidermoid (teratoma with ectodermal elements only)
- burned out testis tumour
- sex cord / stromal tumours of the testis
- testicular cyst
- testicular lymphoma
- bilateral testicular lesion
- paratesticular lesions
- epididymis
- other
- polyorchidism
- cryptorchidism
- tubular ectasia of the rete testis
- cystadenoma of the rete testis
- testicular sarcoidosis
- testicular tuberculosis
- spermatic cord
- fibrous pseudotumour of the scrotum
- scrotal leiomyosarcoma
- testicular adrenal rest tumours (TARTs)
- tunica vaginalis testis mesothelioma
- splenogonadal fusion
- testicular vasculitis
- abnormal testicular Doppler flow (differential)
-
unilateral testicular lesion
- penis
- prostate gland
- KUB
- kidneys
- normal renal anatomy
- hydronephrosis
- urolithiasis
- renal masses
- renal cystic disease
- renal infection
- vascular
- trauma
- ureter
- normal ureter anatomy
- ureteral stricture
- ureteral dilatation
- ureteral anomalies
- ureteral tumours
- ureteral trauma
- other
- bladder
- kidneys








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.