Vestibular schwannoma
Updates to Article Attributes
An acousticAcoustic schwannoma is a relatively common type of tumour which arises from the vestibulocochlear nerve (CN VIII). Bilateral acoustic schwannomas are strongly suggestive of neurofibromatosis type 2 (NF2).
Epidemiology
They account for 7-8% of all primary intracranial tumours 2and 75-90% of cerebellopontine angle masses 1-2,8. Bilateral vestibular schwannomas are highly suggestive of neurofibromatosis type 2 (NF2), although bilateral tumours are encountered in the familial form of acoustic schwannomas in the absence of other stigmata of NF2 5.
Clinical presentation
The typical presentation is with sensorineural hearing loss or tinnitus. In some patients this goes unnoticed and presentation is delayed until the lesion is much larger and presents with mass effect. Possibilities include cerebellar and brainstem symptoms (e.g. other cranial nerve dysfunction), or hydrocephalus due to effacement of the fourth ventricle.
Pathology
Acoustic schwannomas are benign tumours, which usually arise from the intracanalicular segment of the vestibular portion of the vestibulocochlear nerve (CN VIII) 2,4, near the transition point between glial and Schwann cells (Obersteiner-Redlich zone) 8 . In over 90% of cases these tumours arise from the inferior division of the vestibular nerve 8.
They are well circumscribed encapsulated masses, which unlike neuromas, arise from but are separate from nerve fibers 7, which they usually splay and displace rather than incorporated.
They can display two types of growth pattern:
-
Antoni A
- elongated cells with cytoplasmic processes arranged in fascicles 7
- little stromal matrix
- Verocay bodies : nuclear free zones of processes lying between regions of nuclear palisading
-
Antoni B
- loose meshwork of cells
- less densely cellular
- microcysts and myxoid change
Radiographic features
Most vestibular schwannomas have an intracanalicular component, and often result in widening of the porus acousticus resulting in the trumpeted IAM sign, which is present in up to 90% of cases 5. In a minorty of cases ( ~20%) they are purely extracanalicular, only abutting the porus acousticus 1,5. Occasionally these tumours with grow laterally through the cochlear or vestibule into the middle ear. Rarely they are small and confined to the labyrinth 4.
Extracanalicular extension into cerebellopontine angle (path of least resistance) can lead to "ice cream cone" appearnace.
Small tumours tend to be solid whereas cystic degeneration seen commonly in larger tumours 2. Haemorrhagic areas may also be seen. Calcification is typically not present.
CT
May show erosion and widening of the internal acoustic meatus. The density of these tumours on non-contrast imaging is variable, and often they are hard to see, especially on account of beam hardening and streak artefact form the adjacent petrous temporal bone.
Contrast enhancement is present, but can be underwhelming, especially in larger lesions with cystic components.
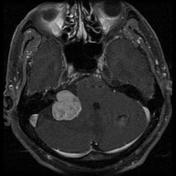
MRI
-
T1
- slightly hypo-intense c.f. adjacent brain - 63%2
- iso intense c.f adjacent brain - 37%2
- may contain hypo intense cystic areas
-
T2
- heterogeneously hyper intense c.f to adjacent brain 5
- cystic areas fluid intensity
- may have associated peri-tumoural arachnoid cysts 3
-
T1 C+ (Gd)
- contrast enhancement is vivid
- but heterogeneous in larger tumours
Post-op MRI
Linear enhancement may not indicate tumour, but if there is nodular enhancement suspect tumour recurrence (needs follow up MRI).
What the surgeon wants to know
In addition to general remarks about the size and location of the tumour, important findings that influence surgical management include 8:
- how close to the fundus of the IAC the tumour reaches
- anatomical variations
- high-riding jugular bulb
- dehiscent jugular bulb
- aberrant ICA
- aberrant course of the facial nerve
- pneumatisation of the petrous apex
- size and location of the sigmoid sinus
Treatment and prognosis
There is variability in the rate of growth of these tumours, and as such the decision to treat requires consideration of patient's age and co-morbidities. The options include 6 :
- sterotactic radiosurgery
- microsurgery - number of approaches are possible, including 8:
- retrosigmoid (trans
meatal-meatal) (suboccipital)- able preserve hearing
- can be used for large tumours
- limited view of the IAC
-
more chanceshas a greater chance of residualtumortumour (in lateral aspect of IAM)
-
middle cranial fossa
- best for small intracanalicular tumours
- able to preserve hearing
- translabyrinthine
- careful skeletonisation of the facial nerve required
- loss of hearing guaranteed
- retrosigmoid (trans
Overall there tumour recurrence is low, ranging between 1 and 9% 8.
Post-op M.R.I :-
- Linear enhancement does not indicate tumor , but if nodular enhancement suspect tumor , needs follow up MRI .
Differential diagnosis
The most frequent differential to be considered are :
-
meningioma
- usually more homogeneous in appearance : significant signal heterogeneity with cystic or haemorrhagic areas is more typical of vestibular schwannoma than meningiomas(although cystic meningiomas do occur)
- meningiomas tend to have a broad dural base
- usually lack trumpet IAM sign
- calcification more common
-
epidermoid
- no enhancing component
- very high signal on DWI
- does not widen the IAM
- metastasis
- uncommon
- usually does not remodel the IAM as metastases are usually present for only a short time
-
ependymoma
- centered on the fourth ventricle
- does not extend into the IAM
- usually younger patients
See also
-<p>An <strong>acoustic schwannoma</strong> is a relatively common type of tumour which arises from the <a href="/articles/vestibulocochlear-nerve">vestibulocochlear nerve (CN VIII)</a>. Bilateral acoustic schwannomas are strongly suggestive of<a href="/articles/neurofibromatosis-type-2-3"> neurofibromatosis type 2 (NF2)</a>.</p><h4>Epidemiology</h4><p>They account for 7-8% of all primary intracranial tumours <sup>2</sup>and 75-90% of <a href="/articles/cerebellopontine_angle">cerebellopontine angle masses</a> <sup>1-2,8</sup>. Bilateral vestibular schwannomas are highly suggestive of <a href="/articles/neurofibromatosis-type-2-3">neurofibromatosis type 2 (</a><a href="/articles/neurofibromatosis-type-2-3">NF2)</a>, although bilateral tumours are encountered in the familial form of acoustic schwannomas in the absence of other stigmata of NF2 <sup>5</sup>. </p><h4>Clinical presentation</h4><p>The typical presentation is with <a href="/articles/sensorineural-hearing-loss-snhl">sensorineural hearing loss</a> or <a href="/articles/tinnitus">tinnitus</a>. In some patients this goes unnoticed and presentation is delayed until the lesion is much larger and presents with mass effect. Possibilities include cerebellar and brainstem symptoms (e.g. other cranial nerve dysfunction), or hydrocephalus due to effacement of the fourth ventricle. </p><h4>Pathology</h4><p>Acoustic schwannomas are benign tumours, which usually arise from the intracanalicular segment of the vestibular portion of the <a href="/articles/vestibulocochlear-nerve">vestibulocochlear nerve (CN VIII)</a> <sup>2,4</sup>, near the transition point between glial and Schwann cells (<a href="/articles/obersteiner-redlich-zone">Obersteiner-Redlich zone</a>) <sup>8</sup> . In over 90% of cases these tumours arise from the <strong>inferior</strong> division of the vestibular nerve <sup>8</sup>. </p><p>They are well circumscribed encapsulated masses, which unlike neuromas, arise from but are separate from nerve fibers <sup>7</sup>, which they usually splay and displace rather than incorporated. </p><p>They can display two types of growth pattern:</p><ol>- +<p><strong>Acoustic schwannoma</strong> is a relatively common type of tumour which arises from the <a href="/articles/vestibulocochlear-nerve">vestibulocochlear nerve (CN VIII)</a>. Bilateral acoustic schwannomas are strongly suggestive of<a href="/articles/neurofibromatosis-type-2-3"> neurofibromatosis type 2 (NF2)</a>.</p><h4>Epidemiology</h4><p>They account for 7-8% of all primary intracranial tumours <sup>2</sup>and 75-90% of <a href="/articles/cerebellopontine-angle-mass">cerebellopontine angle masses</a> <sup>1-2,8</sup>. Bilateral vestibular schwannomas are highly suggestive of <a href="/articles/neurofibromatosis-type-2-3">neurofibromatosis type 2 (</a><a href="/articles/neurofibromatosis-type-2-3">NF2)</a>, although bilateral tumours are encountered in the familial form of acoustic schwannomas in the absence of other stigmata of NF2 <sup>5</sup>. </p><h4>Clinical presentation</h4><p>The typical presentation is with <a href="/articles/sensorineural-hearing-loss-snhl">sensorineural hearing loss</a> or <a href="/articles/tinnitus">tinnitus</a>. In some patients this goes unnoticed and presentation is delayed until the lesion is much larger and presents with mass effect. Possibilities include cerebellar and brainstem symptoms (e.g. other cranial nerve dysfunction), or hydrocephalus due to effacement of the fourth ventricle. </p><h4>Pathology</h4><p>Acoustic schwannomas are benign tumours, which usually arise from the intracanalicular segment of the vestibular portion of the <a href="/articles/vestibulocochlear-nerve">vestibulocochlear nerve (CN VIII)</a> <sup>2,4</sup>, near the transition point between glial and Schwann cells (<a href="/articles/obersteiner-redlich-zone">Obersteiner-Redlich zone</a>) <sup>8</sup> . In over 90% of cases these tumours arise from the <strong>inferior</strong> division of the vestibular nerve <sup>8</sup>. </p><p>They are well circumscribed encapsulated masses, which unlike neuromas, arise from but are separate from nerve fibers <sup>7</sup>, which they usually splay and displace rather than incorporated. </p><p>They can display two types of growth pattern:</p><ol>
-</ul><h5>What the surgeon wants to know</h5><p>In addition to general remarks about the size and location of the tumour, important findings that influence surgical management include <sup>8</sup>:</p><ul>- +</ul><h6>Post-op MRI </h6><p>Linear enhancement may not indicate tumour, but if there is nodular enhancement suspect tumour recurrence (needs follow up MRI).</p><h5>What the surgeon wants to know</h5><p>In addition to general remarks about the size and location of the tumour, important findings that influence surgical management include <sup>8</sup>:</p><ul>
-<li><a href="/articles/high_riding_jugular_bulb">high-riding jugular bulb</a></li>-<li><a href="/articles/dehiscent_jugular_bulb">dehiscent jugular bulb</a></li>-<li><a href="/articles/aberrant_internal_carotid_artery">aberrant ICA</a></li>- +<li><a href="/articles/high-riding-jugular-bulb">high-riding jugular bulb</a></li>
- +<li><a href="/articles/dehiscent-jugular-bulb">dehiscent jugular bulb</a></li>
- +<li><a href="/articles/aberrant-internal-carotid-artery">aberrant ICA</a></li>
-<li>retrosigmoid (trans meatal) (suboccipital)<ul>- +<li>retrosigmoid (trans-meatal) (suboccipital)<ul>
-<li>more chances of residual tumor (in lateral aspect of IAM) </li>- +<li>has a greater chance of residual tumour (in lateral aspect of IAM) </li>
-</ul><p>Overall there tumour recurrence is low, ranging between 1 and 9% <sup>8</sup>.</p><h5>Post-op M.R.I :- </h5><p>- Linear enhancement does not indicate tumor , but if nodular enhancement suspect tumor , needs follow up MRI .</p><h4>Differential diagnosis</h4><p>The most frequent differential to be considered are :</p><ul>- +</ul><p>Overall there tumour recurrence is low, ranging between 1 and 9% <sup>8</sup>.</p><h4>Differential diagnosis</h4><p>The most frequent differential to be considered are :</p><ul>
-<li>usually more homogeneous in appearance : significant signal heterogeneity with cystic or haemorrhagic areas is more typical of vestibular schwannoma than meningiomas<a href="/articles/meningioma"> </a>(although <a href="/articles/cystic_meningioma">cystic meningiomas</a> do occur) </li>- +<li>usually more homogeneous in appearance : significant signal heterogeneity with cystic or haemorrhagic areas is more typical of vestibular schwannoma than meningiomas<a href="/articles/meningioma"> </a>(although <a href="/articles/cystic-meningioma">cystic meningiomas</a> do occur) </li>
-<li><a href="/articles/cerebellopontine_angle">cerebellopontine angle masses</a></li>-<li><a href="/articles/trigeminal_schwannoma">trigeminal schwannoma</a></li>- +<li><a href="/articles/cerebellopontine-angle-mass">cerebellopontine angle masses</a></li>
- +<li><a href="/articles/trigeminal-schwannoma">trigeminal schwannoma</a></li>
References changed:
- 10. Fortnum H, O'Neill C, Taylor R et al. The Role of Magnetic Resonance Imaging in the Identification of Suspected Acoustic Neuroma: A Systematic Review of Clinical and Cost Effectiveness and Natural History. Health Technol Assess. 2009;13(18):iii-iv, ix. <a href="https://doi.org/10.3310/hta13180">doi:10.3310/hta13180</a> - <a href="https://www.ncbi.nlm.nih.gov/pubmed/19358774">Pubmed</a>
Image 5 MRI (T2) ( create )
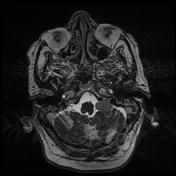
Image 21 MRI (T1 C+) ( update )

Image 23 CT (C+) ( update )

Image 28 MRI (T2_AX THIN) ( create )

Image 29 MRI (Ax T1 -THINS C+ FAT SAT) ( create )