Acute disseminated encephalomyelitis (ADEM): Anti-NMDA receptor encephalitis
Presentation
25 year old presents with a few days history of first episode psychosis, fecal incontinence and auditory-visual hallucination. MRI spine appears unremarkable.
Patient Data
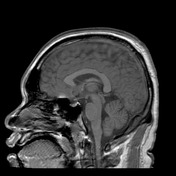
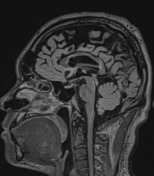
First MRI with contrast: Acute
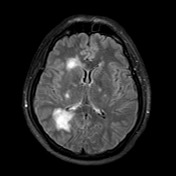





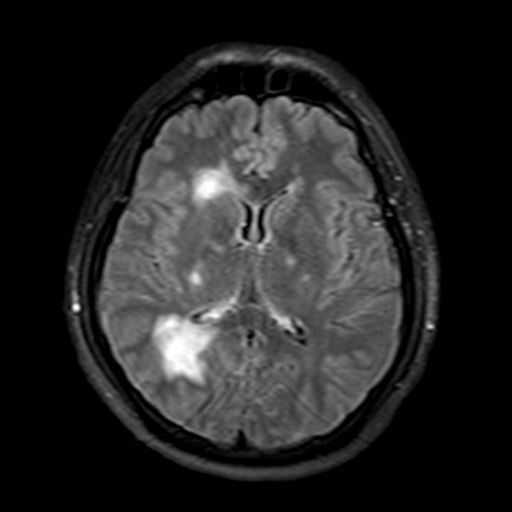
Multifocal bilateral high T2 signal changes in the periventricular deep white matter and bilateral basal ganglia with surrounding vasogenic edema.
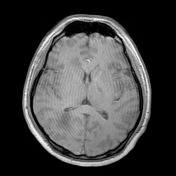
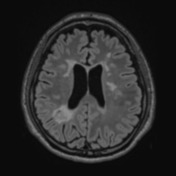
First MRI with contrast: Acute
Post-contrast injection demonstrates abnormal enhancement of the nodular FLAIR lesions.
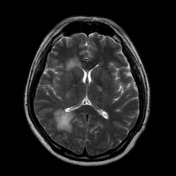
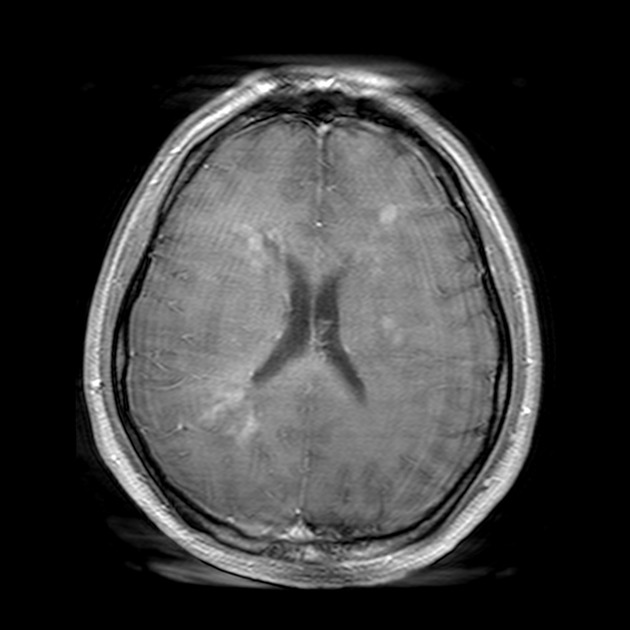
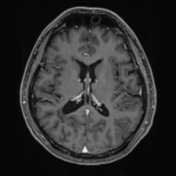
2nd MRI C+: 7 days post Rx...
2nd MRI C+: 7 days post Rx IV methyprednisolone & immunoglobulin cyclophosphamide
After 7 days of treatment, the post-contrast T1 enhancement in the nodular lesions resolved.
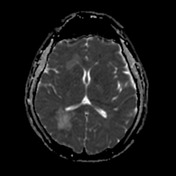
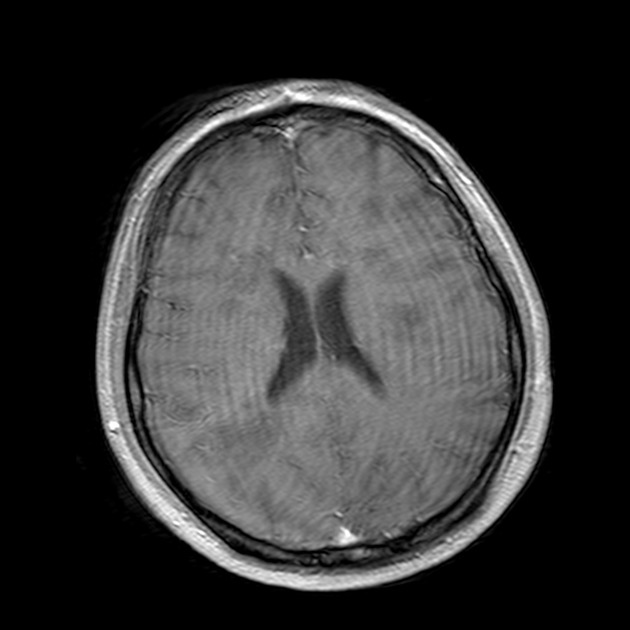
Follow-up MRI 5 years later



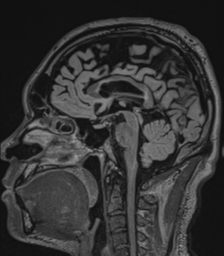
Unchanged periventicular white matter nodular FLAIR-hyperintense lesions compared to five years earlier. Subtle marginal intensities around the nodules are likely due to technical differences. No optic nerve involvement.
Case Discussion
Case Discussion
The patient had anti-NMDA receptor autoantibody presenting with ADEM, which responded well to IV methylprednisolone and immunoglobulin, as well as cyclophosphamide. Due to the extent of the ADEM, he frequently represented with intermittent cognitive and behavioral disturbances. However, the recent MRI and CSF anti-NMDA titer, five years later, demonstrated no signs of relapse.
Anti-NMDA Receptor Discussion
Anti-NMDA receptor encephalitis is a form of cell surface/synaptic, as oppose to intraneuronal, autoimmune disorder.
Features
The first cases of anti-NMDA are a triad of paraneoplastic encephalitis, psychiatric symptoms, hypoventilation in 4 young female with an ovarian teratoma, negative antineuronal antibodies in CSF and serum (Vitaliani, 2005).
Common clinical presentation include psychosis in adults, dyskinesia in children, seizures, catatonia (negativism/paradoxical responses), autonomic dysfunction, hypoventilation, and coma.
Effect of NMDA receptor antagonist agent, Ketamine, causes perceptual disturbances, ideas of reference, paranoid thoughts and executive cognitive deficits in low doses; and psychosis, agitation, memory deficits, motor stereotypi, reduce pain response at high dose; dissociative anesthesia, altered consciousness, catatonia at very high dose. Similar clinical pictures are also seen with phencyclidine (PCP).
Prevalence ranges from 1-4% in clinically undetermined encephalitis cases (Pruss, 2010; Titulaer, 2013), neuropsychiatric (e.g. behavioral disturbance) presentation occurs in over 90%. The peak age of onset is 18-23 years old (range 1-85 years old).
Associations
Neoplasm: 58% women 18-45 years has teratoma. Older men/women may have other carcinomas.
Viral-mediated: 20% Herpes Simplex Encephalitis (Deep cervical LN) develop anti-NMDA receptor antibodies. Some children with post-herpes encephalopathy also develop choreoathetosis and behavioral disturbance. Other autoantibodies may also be present (e.g. GABA-a & dopamine receptors).
Demyelination: 3% has MRI or clinical features of demyelination syndrome (optic neuritis, ADEM, myelitis, brainstem dysfunction), many positive for either aquaporin-4 or myelin oligodendrocyte glycoprotein (Titulaer, 2014).
Pathogenesis
Antigen, released by a tumor, is taken up by antigen-presenting cells, which then transport the antigen to the memory B cells to the lymph nodes for (auto)antibody production. The memory B cells cross the blood-brain barrier and undergo maturation into autoantibody-producing plasma cells, which are long-lived (months-years) and may be refractory to current immunotherapy (e.g. IVIg, Rituximab, plasma exchange). As the plasma cells are protected by blood-brain barrier, the antibody titers in CSF is often higher than in serum.
The pathogenesis is not of a direct antagonism of NMDA receptor. The autoantibody selectively binds, in a crosslink/capping manner, to the NMDA receptor cluster at the GluN1 (NR1) subunit. The autoantibody-receptor complex is then internalised (endocytosis) into the neuron, leading to a loss of surface NMDA receptors at the post-synaptic neuron and compromising their transmission, without affecting other types of receptors (e.g. AMPA) or neuronal viability in the early stages. The latter factor suggests the reversibility of anti-NMDA encephalopathy. The autoantibody also disrupts the post-synaptic interaction between NMDA receptor and Ephrin B2 receptor (which stabilizer of NMDA receptor integrity), leading to the displacement of the NMDA receptors from the synapses. The pathological process also correlates moderately and inversely with CSF antibody titers in rats (Hughes, 2010).
The reduced NMDA activity leads to the hyperdopaminergic state from rapid firing of pyramidal hippocampal cells and reduced inhibitory tone in ventral tegmental area. The hypofunctional NMDA hypothesis has also been associated in Schizophrenia.
Histology may show mild inflammatory infiltrate and neuronal loss, microglia activation, and IgG deposits without complement.
EEG
30% of patients may have 'extreme delta brush' (delta wave superimposed on beta activity) pattern in a continuous EEG monitoring, which is associated with longer hospitalization (Schmitt, 2012).
Radiology
MRI can appear unremarkable in 50% of cases (Delmau, 2011). Hippocampal T2/FLAIR hyperintensities may be seen on MRI. Other non-specific hyperintensities may be seen in other areas of the brain and spine. Hippocampal atrophy appears to correlate with memory impairment, more severe and longer onset in post-acute cohort (Finke, 2016).
Treatment
Typical first line treatment is a combination of IV Immunoglobulin and methyprednisolone. Other treatments include plasmapheresis, rituximab and cyclophosphamide.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.