Presentation
Spastic tetraparesis progredient over months. Ankle clonus. Atrophy of the small hand muscles. Fasciculations in all extremities. Dysarthria. Positive palmomental reflex. Pathological laughter and yawning.
Patient Data


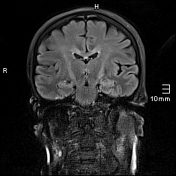

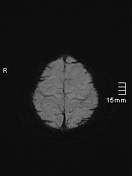

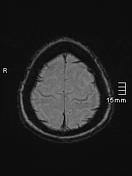

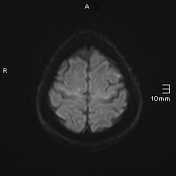

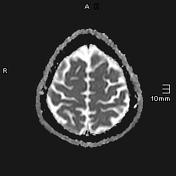

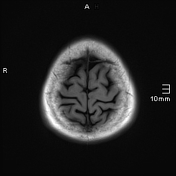

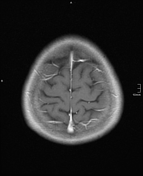

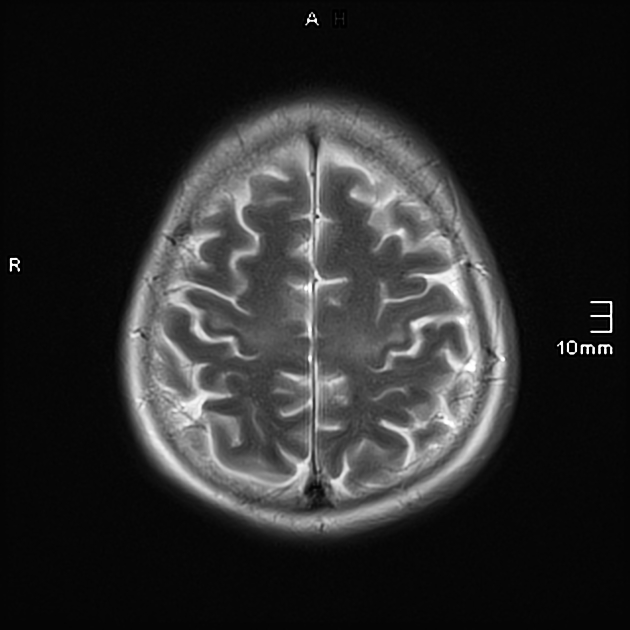
T2/FLAIR hyperintensity in the precentral gyrus and corticospinal tracts bilaterally. Cortical SWI hypointensity in the precentral gyrus bilaterally, known as the motor band sign.
Case Discussion
This case demonstrates imaging from a patient with clinically established amyotrophic lateral sclerosis (ALS). The diagnosis of classic ALS was established upon meeting the Escorial criteria for clinically definite ALS 1:
- signs of upper motor neurone damage (spastic pareses progredient over time, hyperreflexia) in >3 regions
- signs of lower motor neurone damage (muscle atrophy, fibrillations/fasciculations in extremities and the tongue, and bulbar paresis (dysarthria, pathological laughter))
- absence of other causes for upper or lower motor neurone damage (e.g. brain MRI as above, spinal canal stenosis was excluded by imaging (not included in this case), EMG was normal, blood and CSF tests were unremarkable)
This case shows two typical MRI signs of ALS:
- T2 hyperintensity in the corticospinal tracts
- motor band sign
It is important to note that these radiological signs are rather unspecific and ALS remains a clinical diagnosis. Further both of these features are frequently seen subtly in 3 T imaging in healthy individuals and thus an appreciation for a 'normal' degree of signal in the corticospinal tract is essential.
In the four years since these images were obtained, the patient's spastic tetraparesis deteriorated, there was progressive atrophy of the extremities and additional troubles breathing. The ALS-FRS (Amyotrophic Lateral Sclerosis Functional Rating Scale) deteriorated from 38 to 19 within those 4 years.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.