Presentation
Out-of-hospital cardiac arrest with ECG findings suggestive of AMI. Catheter angiogram confirmed a lesion in the left anterior descending (LAD) artery, treated with balloon angioplasty. Subsequent echocardiogram revealed mitral valve vegetations and signs of endocarditis. The patient exhibited a low Glasgow Coma Scale (GCS) score after the procedure.
Patient Data

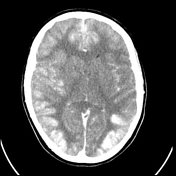
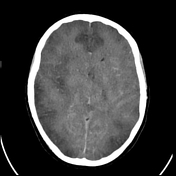
It is noted that images have been obtained in close proximity to coronary angiography, precluding an accurate non-contrast study.
There is extensive hyperattenuation throughout the bilateral cerebral hemispheres, predominantly involving the cortex and subcortical white matter. Hyperattenuation is also observed throughout the dural venous sinuses and cerebral arteries. No evidence of leptomeningeal enhancement is found. Virtual non-contrast reconstructions (not available) show no definite intracranial haemorrhage. Mild generalised sulcal effacement and effacement of the lateral ventricles are noted, with no midline shift or herniation. No enhancing focal masses are identified.
Impression:
Hyperattenuating regions throughout the brain are favoured to represent enhancement, likely due to contrast from the recent cardiac angiography, rather than haemorrhage. The enhancement in these regions is nonspecific; however, in the context of possible endocarditis and recent CPR, these findings may indicate sequelae of cerebritis or acute cerebral ischaemia.


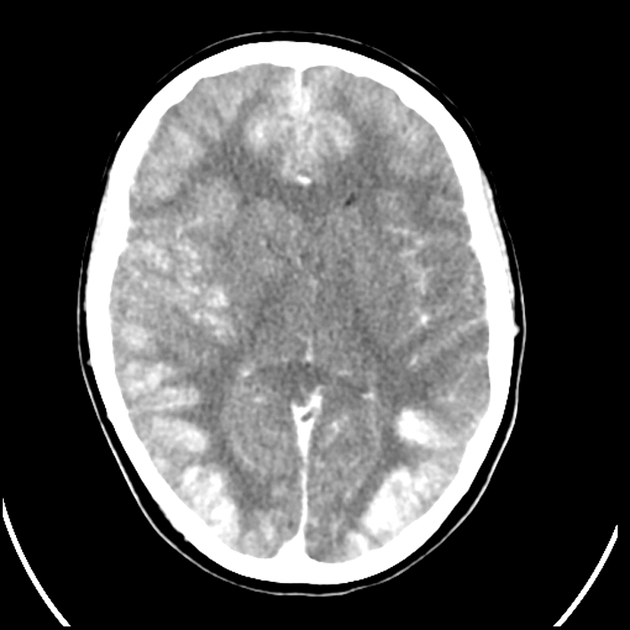
Diffuse progressive cerebral oedema with effacement of the sulcal spaces, near-complete effacement of the right lateral ventricle more than the left, and effacement of the suprasellar cistern. A 4 mm left midline shift and mild right subfalcine herniation are observed. Although there is no uncal herniation, the cerebrum is pressed down over the tentorium cerebelli. Kinking of the cervical medullary junction and effacement of the pre-pontine cisterns are noted. No cerebellar tonsillar herniation is observed, and there is preserved fourth ventricle calibre.
Diffuse patchy cortical enhancement is seen, secondary to previous contrast administration in the context of diffuse cerebral cortical ischaemia, loss of blood-brain barrier, and reperfusion, possibly associated with diffuse cortical necrosis. The majority of this hyperdensity suppresses on the virtual non-contrast spectral data, which also demonstrates a reversal of the normal grey-white matter differentiation.
Conventional CT reveals a loss of grey-white matter differentiation in the temporal lobes, bilateral frontal lobes, and posterior parietal lobes.
The dural venous sinuses and the Circle of Willis are opacified, likely secondary to the recirculation of iodinated contrast that has not been cleared due to suspected progressive acute kidney injury.
Mucosal thickening is noted in the left maxillary sinus.
Impression:
Diffuse cerebral oedema with mass effect as described. Diffuse cortical ischaemia with a suspected infarct and cortical necrosis. Imaging appearances are accentuated by the recirculation of iodinated contrast from suspected progressive acute renal injury.
Case Discussion
The patient died in the ICU.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.