Presentation
Preoperative endometriosis mapping. Prior laparotomy showed bowel adhesions, obliterated pouch of Douglas, salpingectomy and endometrioma. Recent transvaginal ultrasound showed bilateral endometrioma, urinary bladder and bowel endometriosis.
Patient Data



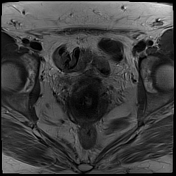



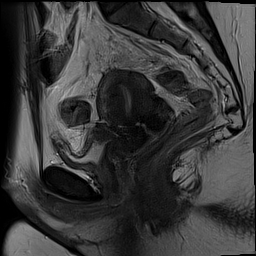
ANTERIOR COMPARTMENT:
Urinary bladder: Posterior dome 18 x 18 x 19 mm (CC x AP X TV) T2 dark thickening with
adjacent distortion obliterating the vesicouterine pouch, a few T1 hyperintense foci consistent with the urinary bladder deep infiltrating endometriosis.
No hydroureter.
MIDDLE COMPARTMENT:
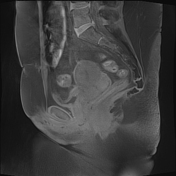
Uterus: Anteverted retroflexed 60 mm in the midline. Morphology normal. Endometrium 5 mm thin and regular. Junctional zone thickening anteriorly 14 mm consistent with adenomyosis. No T2 or T1 hyperintensities. No myometrial lesion. Posterior uterine/torus 20 x 3 mm linear T2 dark thickening/distortion tethering the upper rectum and obliterating the Pouch of Douglas. Mobility: fixed.
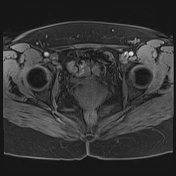
Left ovary 45 mm, was 52 mm, unilocular T2 shaded cyst, not T1 bright. Wall thin and regular. No septa or solid part. Likely a resolving hemorrhagic corpus luteal follicle. Ipsilateral unilocular 10 mm and 7 mm T1 bright cysts, endometriomata. Contralateral 14 mm unilocular and 10 mm unilocular T1 bright cysts, endometriomata. Mobility fixed.
Bilateral salpingectomy, no residual tube seen.
POSTERIOR COMPARTMENT:
At the torus, and uterine fundus there is multi-focal superficial tethering of the rectosigmoid to the uterus.
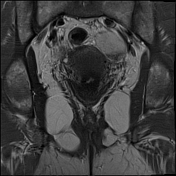
Superior to the urinary bladder is a 40 x 14 mm typical mushroom-shaped bowel endometriosis involving the sigmoid colon, best seen on coronal images. The surrounding bowel is distorted.
At the right adnexa, fixed to the right ovary is a 37 x 9 mm sigmoid bowel endometriosis.
An adjacent 30 mm segment of asymmetric sigmoid thickening may represent further bowel endometriosis.
Case Discussion
This MRI shows typical endometriosis in all three compartments with a typical mushroom-shaped sigmoid bowel endometriosis (best seen on coronal T2).




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.