Presentation
General malaise, raised inflammatory markers, splinter haemorrhages, and Osler nodes. Initially, there was a strong suspicion of infective endocarditis, but initial blood cultures and transthoracic echocardiogram were negative. History of aortic valve replacement several months previously.
Patient Data






Midline sternotomy and bioprosthetic aortic valve replacement.
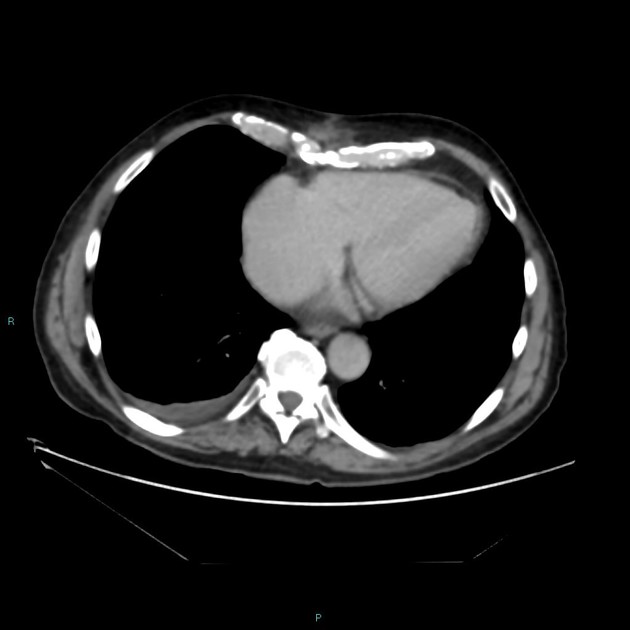
4.5 cm filling defects within the lumen of the ascending aorta, extending from the aortic valve superiorly. Mural oedema was seen along the anterior aortic root and extending into the anterior mediastinum, with a 3 cm max diameter walled-off collection seen adjacent (to the right of the midline).
Ground glass changes and interstitial thickening in the right upper lobe are presumed reactive.
Right pleural effusion.
Several prominent but subcentimetre mediastinal lymph nodes.
No other significant findings.
Case Discussion
Large lobular filling defects seen on CT in keeping with vegetations of infective endocarditis. These were not seen on transthoracic echocardiogram (possibly due to metal artifact), but were later also demonstrated on transoesophageal echocardiogram.
Blood cultures were initially negative but repeated cultures and further testing later demonstrated Aspergillus galactomannan. Impression was that this was therefore likely a case of fungal endocarditis.
Fungal endocarditis is uncommon but carries a poor prognosis. Vegetations are often large at diagnosis and rates of embolisation are very high 1. It is not only difficult to diagnose but also difficult to treat.



 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.