Presentation
The patient was found on the floor at home. On examination, she was confused with a reduced level of consciousness and fever.
Patient Data

There is a right frontal laceration with regional soft tissue swelling, subgaleal haematoma with overlying gauze, and associated artifact. This corresponds to the site of impact on fall. The cranium was intact on bony windows. There is a subtle low-density appearance within the left temporal lobe and insular cortex. There are attenuated left temporal surface sulci and Sylvian fissure. There are no post-traumatic surface collections, no subarachnoid haemorrhage, no contusions, and no intracerebral haemorrhage. There is age-appropriate involutional change.















There is T2 and T2 FLAIR high signal intensity within the affected left anterior and anteromedial temporal lobe and insular cortex. There is mixed restriction and shine through on ADC mapping. There is no associated haemorrhage or blooming on the respective T1 and Gradient Echo sequences. There is no midline shift. There is minimal non-specific microvascular ischaemic change.














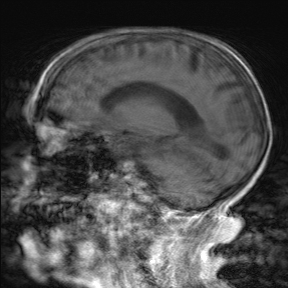
There is a progressive left temporal lobe oedema and involvement with an improved appearance on diffusion imaging. There is new identification of anterior and anteromedial, left temporal lobe haemorrhage on T1 and Gradient Echo sequencing with sedimented blood within the posterior temporal horns.
Case Discussion
A confirmed case of HSV-1 encephalitis on lumbar puncture. One can easily offer acute infarction as a possible diagnosis based on the initial CT and MRI brain studies. There is a wide differential diagnosis including limbic encephalitis, gliomatosis cerebri, status epilepticus, and infective encephalitis. The spiking fevers in this patient and positive lumbar puncture confirmed HSV-1 encephalitis.
Although the follow-up MRI demonstrates a restless and ill patient with associated unavoidable motion artifact, the limited imaging does offer information assisting the ongoing management of the patient.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.