Presentation
Premature birth, intubation and insertion of umbilical catheters.
Patient Data
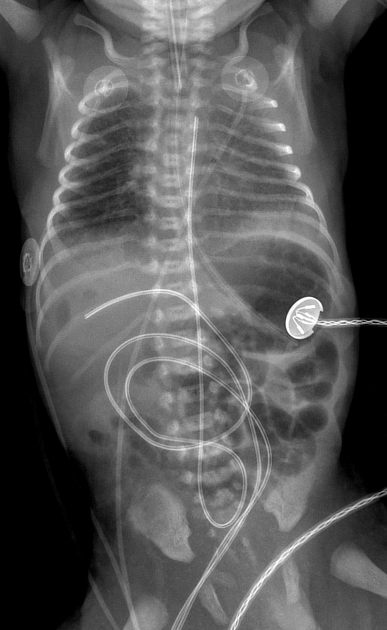
The lung fields are reasonably inspired with surfactant deficiency disorder.
Central trachea. Ill-defined and magnified cardiomediastinal contour with respiratory motion at the time of exposure.
The ET tube is a T1/T2 vertebral body level and appears satisfactorily sited.
The nasogastric tube is satisfactorily sited.
The umbilical venous catheter (UVC) is within a branch of the right portal vein, with suspicious intrahepatic lucencies.
The umbilical arterial catheter (UAC) appears high riding with the tip at approximately T3 vertebral body level and should be retracted 2cm.
Overlying triple ECG leads.
Overlying temperature lead.
Humeral ossification centers are absent, suggesting prematurity radiologically, consistent with referral history.
There are twelve pairs of ribs.
Bones and soft tissues appear otherwise normal.


The portable ultrasound confirms the presence of linear, peripheral echogenicities consistent with gas within the branches of the right portal vein. There is no irregular fluid collection, no TPNoma and no intrahepatic abscess formation. The upper abdominal ultrasound is otherwise unremarkable.
Case Discussion
Features consistent with peripheral portal venous gas in a setting of a malpositioned UVC within a branch of the right portal vein. In this instance, the gas is related to the insertion and use of the umbilical venous catheter, i.e. exogenous gas.
Necrotizing enterocolitis needs to be definitively excluded in cases of portal venous gas.
The portable X-ray was performed within 30 minutes of birth and insertion of the tubes and catheters. This further affirmed the portal venous gas to be likely exogenous and related to umbilical catheterization. A hepatic abscess at birth would be extremely unlikely. There is confirmation of dextrose saline infusion, while TPN was to be started after 24 hours and confirmation of a satisfactorily sited UVC.
Ultrasound confirmed the absence of intrahepatic fluid collection/abscess/TPNoma.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.