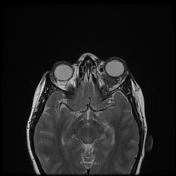
Orbital cavernous venous malformation complicated by spontaneous hemorrhage
Presentation
A 25-year-old female 5 months pregnant presented with sudden left eye proptosis and pain.
Patient Data
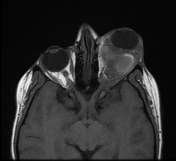

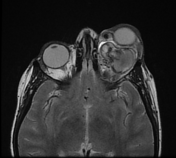

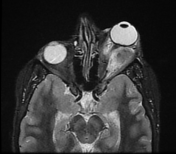


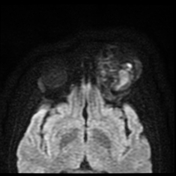

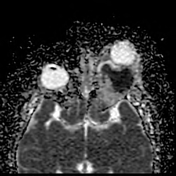

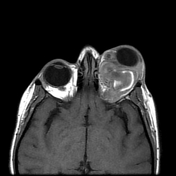

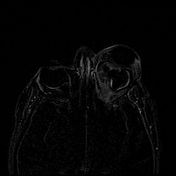

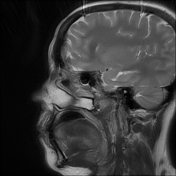

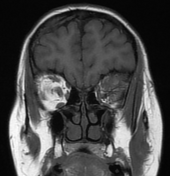

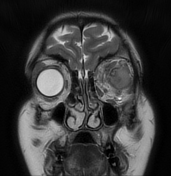


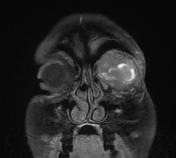

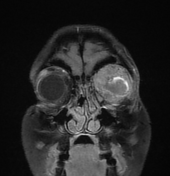

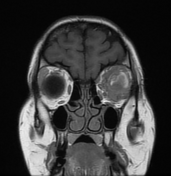


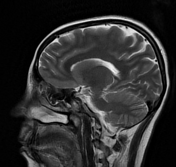

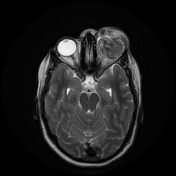

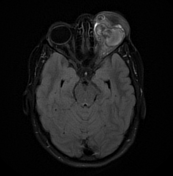


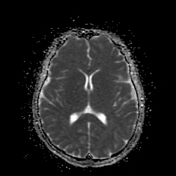

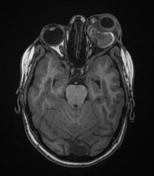



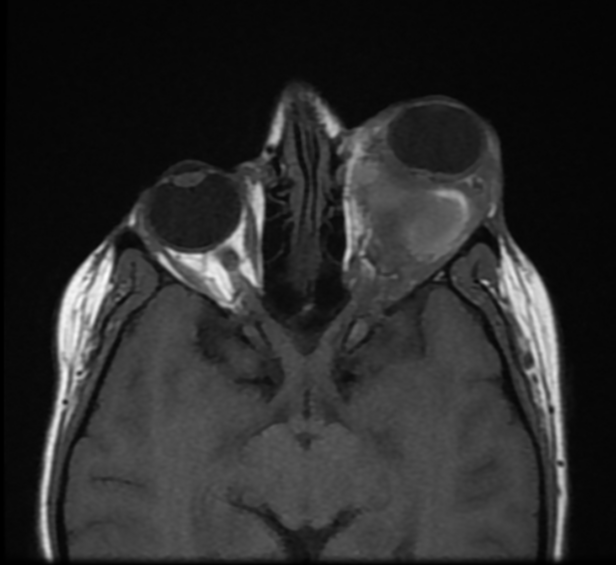
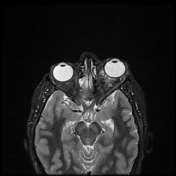
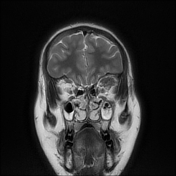
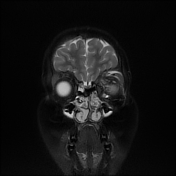
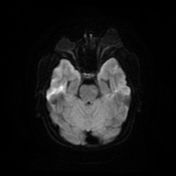
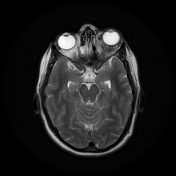
Left intra-orbital intra-conal retrobulbar hemorrhagic lesion with anterior preseptal extension. The lesion displaces the left eye globe anteriorly. It displaces the optic nerve inferiorly and the adjacent recti muscles laterally. It measures roughly about 4.8x3.7x3.2 cm along its max AP, Ts and CC diameters respectively. It elicits heterogeneous signal with internal areas of blood signal being of high T1 signal and causing a blooming effect on SWI. Faint contrast enhancement is seen around the hemorrhagic lesion, also with adjacent prominent small feeding vessels. A small calcific focus is seen at the inner canthus.
Radiological findings are suggestive of complicated (bleeding) cavernous venous malformation.

On CT, it appears as a hyperdense hemorrhagic lesion with phlebolith seen at the inner canthus, confirming the possibility of bleeding vascular malformation.


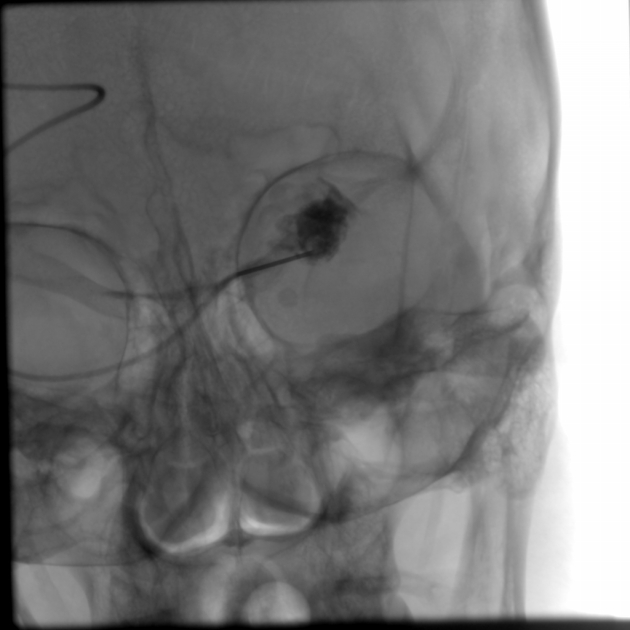
Digital subtraction angiography revealed pooling of contrast in the lesion.
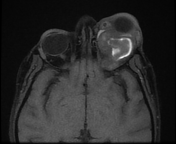
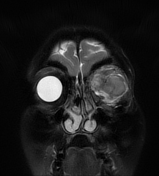
After 1 session of embolizatin


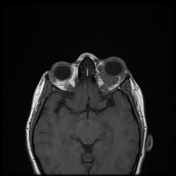

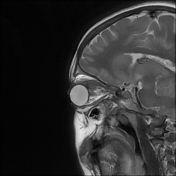



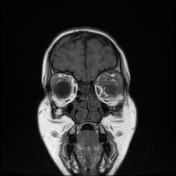



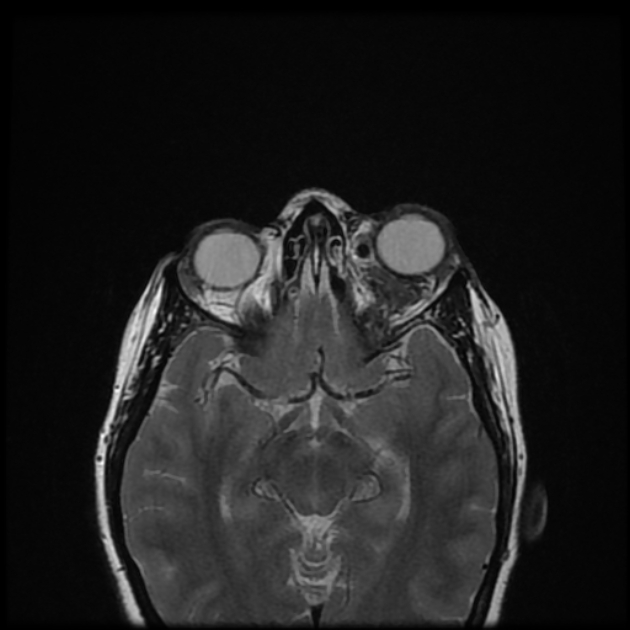
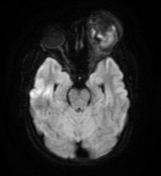
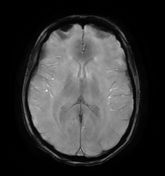
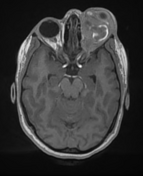
MRI of the orbits after 1 session of embolization showed marked size regression of the malformation and the accompanying hematoma.
Case Discussion
Our patient presented with acute proptosis secondary to acute spontaneous rupture of cavernous hemangioma with subsequent intra-orbital hemorrhage. The patient was treated with three subsequent sessions of embolization of the lesion with significant clinical improvement.
Cavernous hemangiomas are the most common vascular lesions of the orbit in adults with a female predilection. They are considered low-flow venous vascular malformation according to the ISSVA classification. Histologically, they consist of dilated vascular channels containing blood and occasional thrombi and lined by flat endothelial cells.
Orbital cavernous hemangioma grows faster and is thought to be susceptible to spontaneous hemorrhage in pregnant women due to hormonal changes 3.
Phleboliths and bony spurs arising from the orbital margin are characteristic of orbital venous anomalies
Spontaneous hemorrhagic rupture of orbital cavernous hemangioma is an extremely rare occurrence 1.
As they disseminate across the trabeculations of the orbital fat and its fine connective tissue, intraorbital hemorrhages are often poorly delimited, giving the radiologic appearance of a diffuse reticular pattern with less clear borders 2.
When an acute orbital process is present, an MRI should be done to confirm the hemorrhage and distinguish it from an orbital tumor. It is preferable to wait with conservative treatment until the hemorrhage is cleared before performing a follow-up CT to confirm the diagnosis once the hemorrhage is confirmed in a suspected orbital venous abnormality. Unnecessary surgical intervention can be prevented in this way 2.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.