Traumatic subarachnoid haemorrhage complicated by cerebral vasospasm
Presentation
Code stroke. Left facial droop. Aphasia.
Patient Data




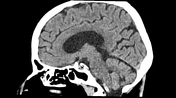


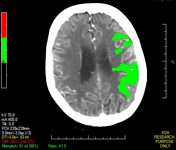
A small volume of left frontal subarachnoid haemorrhage. A tiny contusion in the left temporal lobe and a further left temporooccipital contusion with adjacent subarachnoid haemorrhage. No mass effect or herniation. Grey-white differentiation is maintained. Periventricular hypoattenuation. Asymmetric left deep white matter hypoattenuation foci may represent ischaemia/infarct. No hydrocephalus or extra-axial fluid collections.
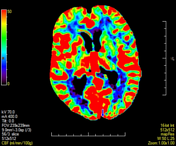

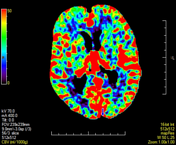

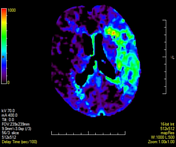


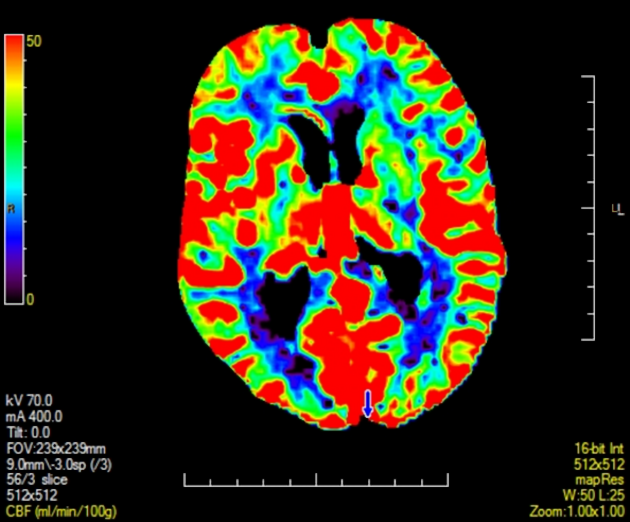
Increased left MCA territory TMax with mainly deep white matter mildly reduced CBV but preserved CBF.
Automated calculations:
Infarct core: 2 mL
Tissue at risk: 83 mL
Mismatch ratio: 41.5




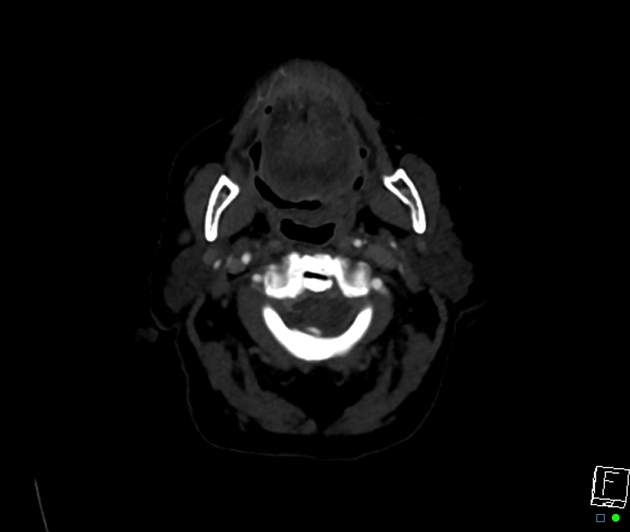
No occlusion or hemodynamically significant stenosis. Terminal left internal carotid artery aneurysm involving the origin of the left middle cerebral artery. The left middle cerebral artery has a markedly smaller calibre than the right, particularly within the M2 division. No further intracranial aneurysm is identified.
Non-united dens fracture (type 2), no marked displacement, although there is a basilar impression.
Case Discussion
The pattern of intracranial haemorrhage is more typical for a traumatic rather than primary intracranial cause. Further history from the referrer was provided of multiple falls during the day prior to the presentation. The intracranial aneurysm is most likely incidental.
The CT perfusion findings in the setting of traumatic subarachnoid haemorrhage most likely represent vasospasm and show that not all mismatches are due to embolic arterial occlusion.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.