Acute aortic syndrome describes the presentation of patients with one of a number of life-threatening aortic pathologies that give rise to similar clinical presentations.
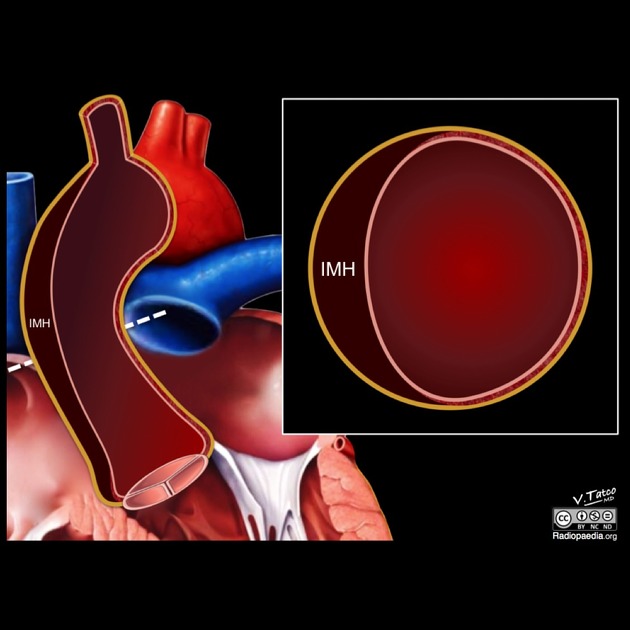
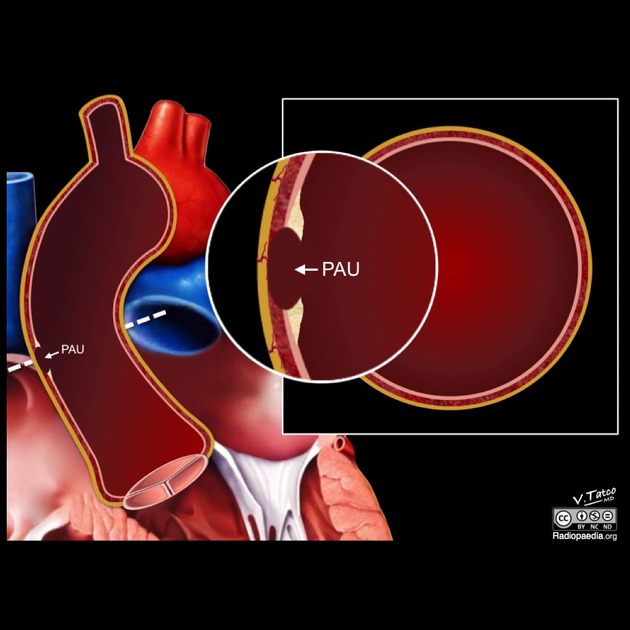
Exactly which entities are included under the umbrella term acute aortic syndrome varies somewhat from publication to publication. Three conditions are generally included, sharing epidemiological and clinical presentation as well as having overlapping and sometimes co-existing imaging features 1-5.
Although some authors also include unstable aortic aneurysmal rupture (leak) and traumatic aortic injury (e.g. thoracic aortic injury and abdominal aortic injury) 1, this article will limit itself to the aforementioned three core conditions.
On this page:
Epidemiology
Generally, patients are elderly, more frequently male and with a long history of hypertension 2,5. Additionally, connective tissue disorders (e.g Marfan syndrome, Ehlers-Danlos syndrome), as well as bicuspid aortic valve and annuloaortic ectasia, are risk factors, particularly for aortic dissection 2,5.
Clinical presentation
Patients will present similarly, with acute "aortic pain" characterised by severe chest pain that has a tearing and sometimes migratory character 2. The location of the pain correlates with the location of pathology. Pain located anteriorly in the chest or in the neck and jaw typically denotes ascending aortic involvement. In contrast, pain in the back and abdomen suggests descending aortic pathology 2. Hypertension is often present.
If the aortic root or ascending aorta is involved, patients may present with shock, hypotension and congestive heart failure 9.
Symptoms may overlap with those of an acute coronary syndrome or pulmonary embolus.
Radiographic features
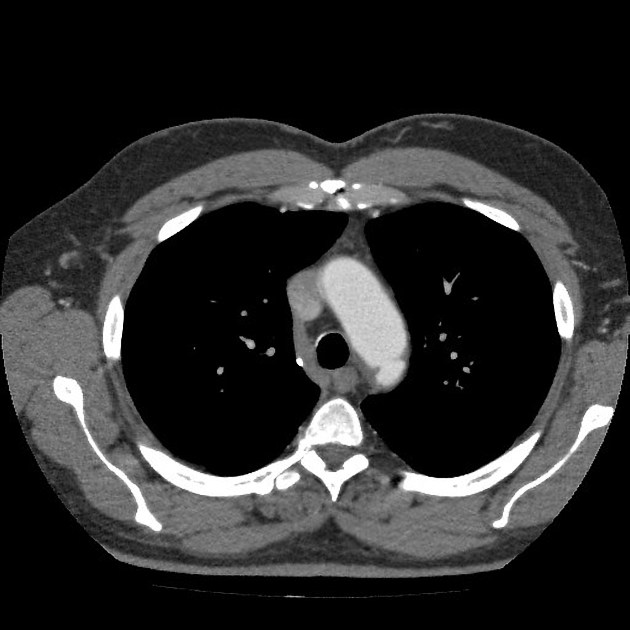
Imaging of patients presenting with suspected acute aortic syndrome in most centres typically involves a CT of the chest as it is readily available, fast to acquire, has been shown to have very high sensitivity and specificity, and is able to image not only the aorta but also the remainder of the neck, chest and abdomen. MRI and transoesophageal echocardiography are also helpful in some situations, however, access is usually more restricted 6.
CT
Although exact imaging parameters will depend on individual and institutional preferences, typically patients are imaged with bi-phasic or tri-phasic CT 6,7.
-
non-contrast:
-
technical considerations:
in low-risk patients or if dual-energy CT with virtual non-contrast imaging is available then the non-contrast phase may be omitted
-
to assess:
hyperdense intramural haematoma
displaced intimal calcification within the lumen of the aorta
differentiate haemopericardium from pericardial effusion 9
-
-
arterial phase:
-
technical considerations:
preferably right arm injection to avoid streak artifact from undiluted contrast in the brachiocephalic vein
3-5 mL/sec flow rate preferred followed by a saline flush 9
non-gated CTA will cause motion (pulsation) artifact of the aortic root but high pitch rates and wider detector arrays can minimise this artifact 9
-
consider cardiac gating, but typically results in higher radiation
removes pulsation artifact of the aortic root and ascending aorta
allows assessment of the coronary arteries that may be involved
retrospective gating allows for the assessment of aortic valve function
-
to assess:
morphology of dissection/ulcer
side-branch patency
-
-
venous phase
-
to assess:
distal organ enhancement/perfusion
-
-
delayed phase 9
Imaging features of individual conditions are discussed separately:
Treatment
The location of the pathology determines the treatment, rather than the type of vascular wall injury. As classically defined and simply put, pathology involving the ascending aorta is treated with emergency open surgery whereas more distal disease sparing the ascending aorta is treated with medical therapy and endovascular stenting.
Complications
Up to 30% of cases of AAS have complications at the time of presentation 8. These include (depending on the type, location and extent of AAS):
rupture
haemopericardium +/- tamponade
aortic valve dysfunction
coronary artery dissection and/or occlusion
aortic branch dissection and/or occlusion
end organ ischaemia or infarction









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.