Adrenal haemorrhage can result from a variety of traumatic and non-traumatic causes. When unilateral, it is often clinically silent. In contrast, bilateral adrenal haemorrhage can lead to catastrophic adrenal insufficiency.
On this page:
Clinical presentation
The clinical signs of adrenal haemorrhage are very non-specific, but can include abdominal pain and secondary signs of significant blood loss such as hypotension or tachycardia 4.
The large majority of patients with unilateral adrenal haemorrhage do not have clinically obvious signs of adrenal insufficiency and the diagnosis is usually made incidentally at imaging performed for another reason.
Bilateral haemorrhage often results in an adrenal crisis, with coma and death resulting if steroid replacement therapy is not administered promptly. Despite treatment, overall there is approximately a 15% mortality, and about 50% when in the setting of sepsis.
Pathology
Adrenal haemorrhage can be either unilateral or bilateral. Adrenal gland trauma is a common cause of unilateral adrenal haemorrhage. On the other hand, bilateral adrenal haemorrhage is rarely due to trauma and is frequently attributed to adrenal vein spasm or thrombosis. Predisposing risk factors include:
- sepsis, especially meningococcaemia (also known as Waterhouse-Friderichsen syndrome)
- disseminated intravascular coagulation (DIC)
- primary antiphospholipid syndrome
- heparin-induced thrombocytopenia
- steroid usage
- anticoagulation
- underlying adrenal tumour
- in neonates (birth trauma, sepsis, hypoxia, adrenal insufficiency, haemorrhagic disorders and diabetic mothers) 7,8
- adrenal vein thrombosis
Adrenal haematoma can be seen in the setting of recent ipsilateral nephrectomy in about 5% of cases 11.
Radiographic features
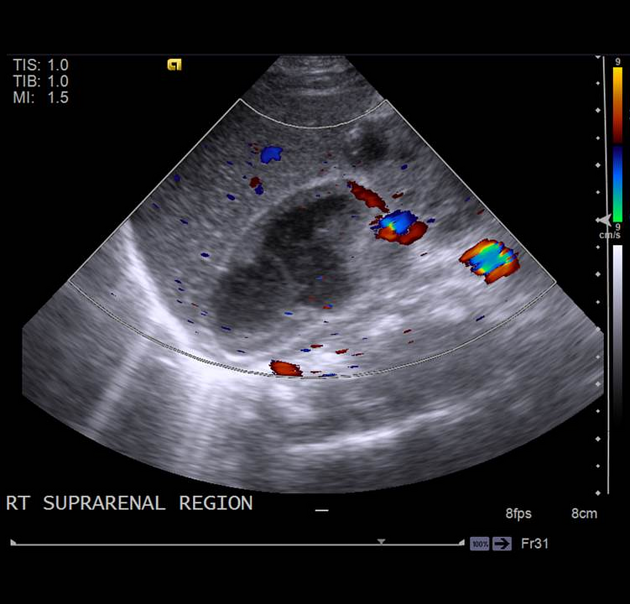
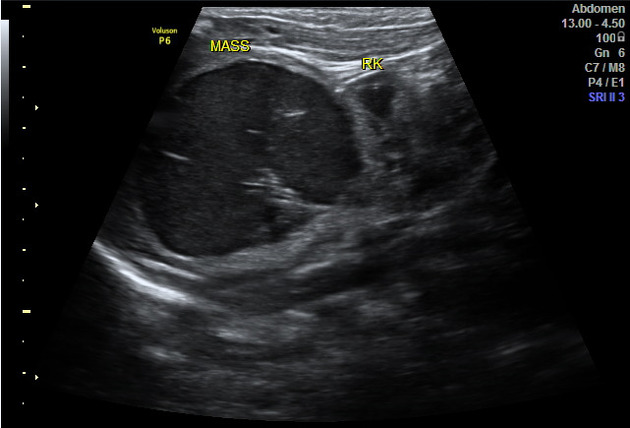
Ultrasound
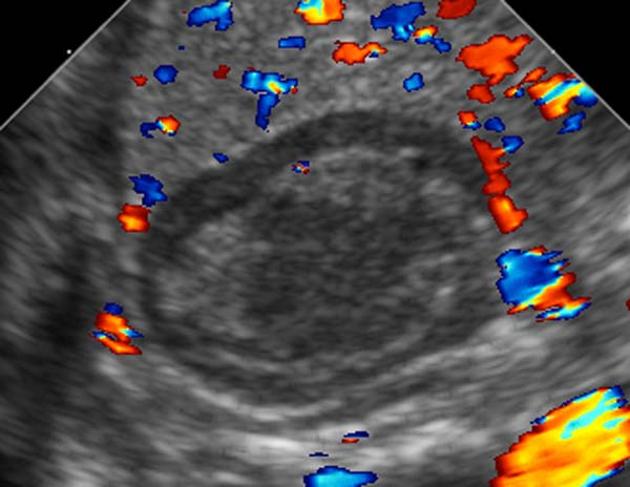
The pattern of echogenicity of an adrenal haematoma depends on its age:
- an early-stage haematoma appears solid with diffuse or inhomogeneous echogenicity
- as liquefaction occurs, the mass demonstrates mixed echogenicity with a central hypoechoic region and eventually becomes completely anechoic and cyst-like
- calcification may be seen in the walls of the haematoma as early as 1-2 weeks after onset and gradually compact as the blood is absorbed
Colour Doppler and power Doppler imaging confirm that the mass is avascular.
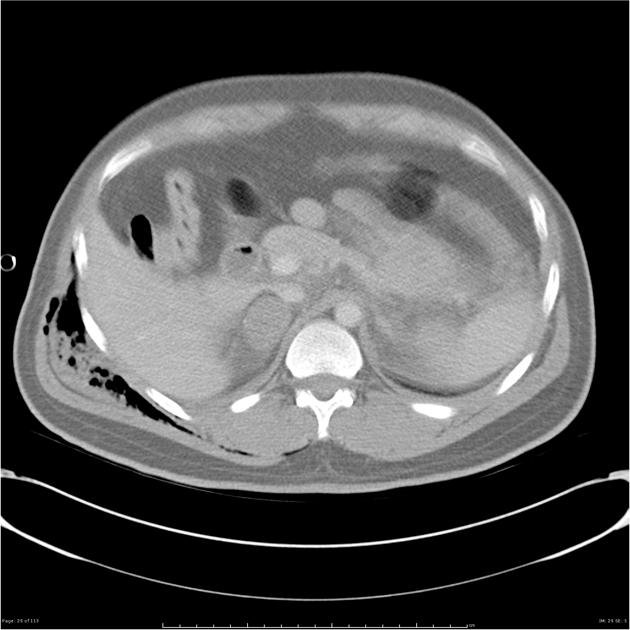
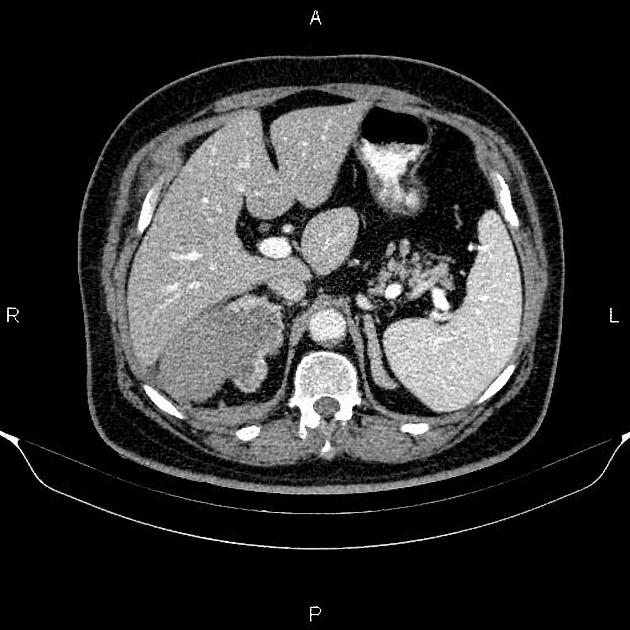
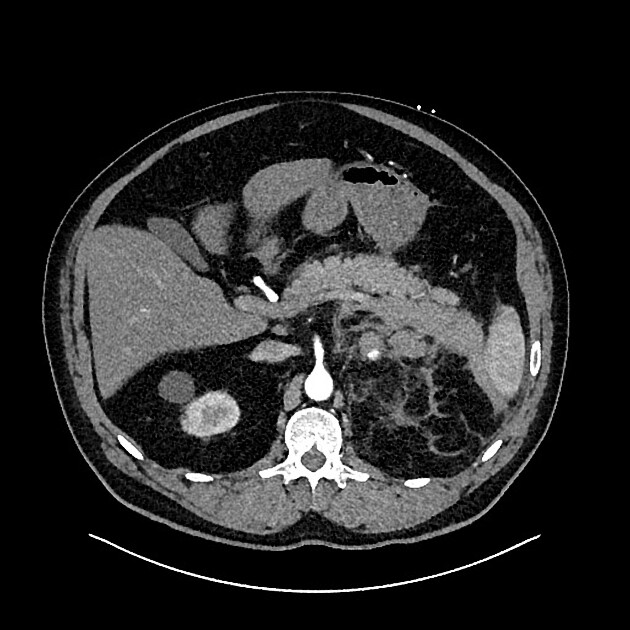
CT
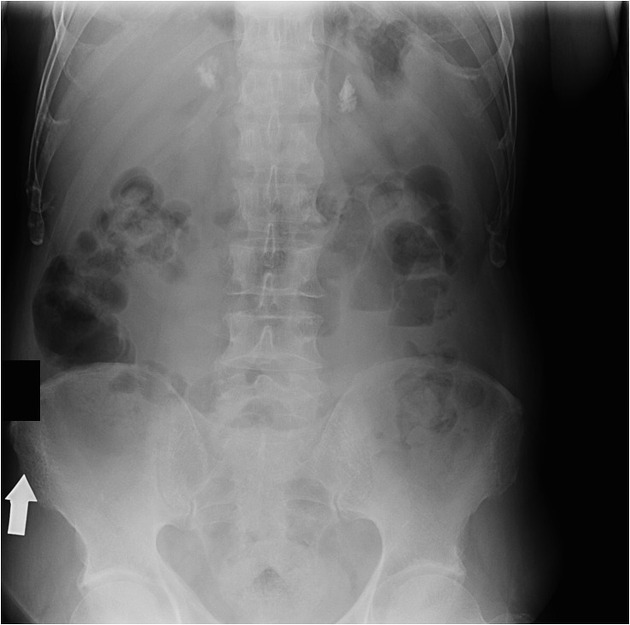
Adrenal haematomas characteristically appear round or oval, often with surrounding stranding of the periadrenal fat.
The attenuation value of an adrenal haematoma depends on its age:
- acute to subacute haematomas contain areas of high attenuation that usually range from 50-90 HU
- adrenal haematomas decrease in size and attenuation over time, and most resolve completely
- organised chronic adrenal haematoma appears as a mass with a hypoattenuating centre, with or without calcifications (also known as adrenal pseudocysts)
- adrenal haematomas may calcify after one year
Of note, adrenal congestion, described as adrenal thickening and peri-adrenal stranding, has been reported to precede adrenal haemorrhage 10, although more research is needed to understand this process.
MRI
- acute stage (<7 days after onset): the haematoma typically appears isointense or slightly hypointense on T1 weighted images and markedly hypointense on T2 weighted images
- subacute stage (7 days to 7 weeks after onset): the haematoma appears hyperintense on T1 and T2 weighted images
- chronic stage (typically >7 weeks after onset): a hypointense rim is present on T1 and T2 weighted images, which is attributed to haemosiderin deposition and the presence of a fibrous capsule
Differential diagnosis
- in neonates
-
neuroblastoma
- liver metastasis
- vascularity
-
congenital adrenal hyperplasia
- bilateral
- glands are enlarged and have a cerebriform contour
-
neuroblastoma
- in adults
- if only limited images of the upper abdomen are available, it may be difficult to differentiate a rim-calcified haematoma from a splenic artery aneurysm






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.