An MR arthrogram is an MRI performed after a joint is injected with a solution containing gadolinium. Sometimes abbreviated to MRA, which can be confused with MR angiography. MRI can also be performed after an injection is not directly administered into the joint, via an indirect arthrogram. An arthrogram also refers to the procedure of injecting a joint.
On this page:
Indications
elbow: partial ulnar collateral ligament (UCL) tear
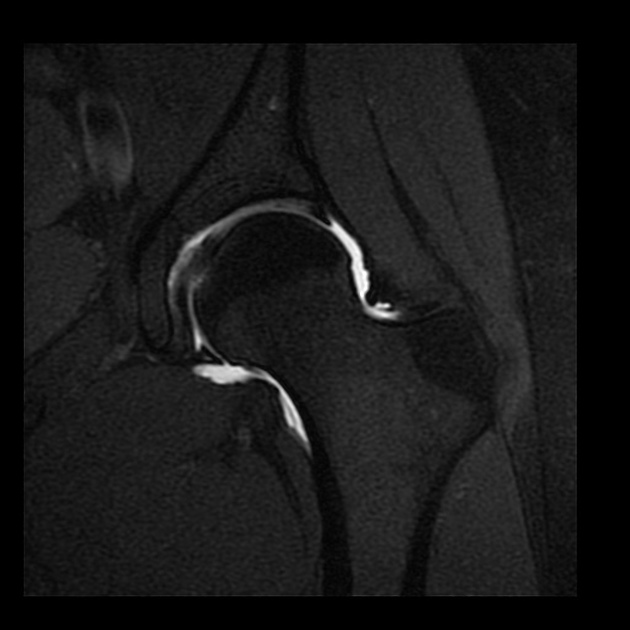
knee: repaired meniscus tears
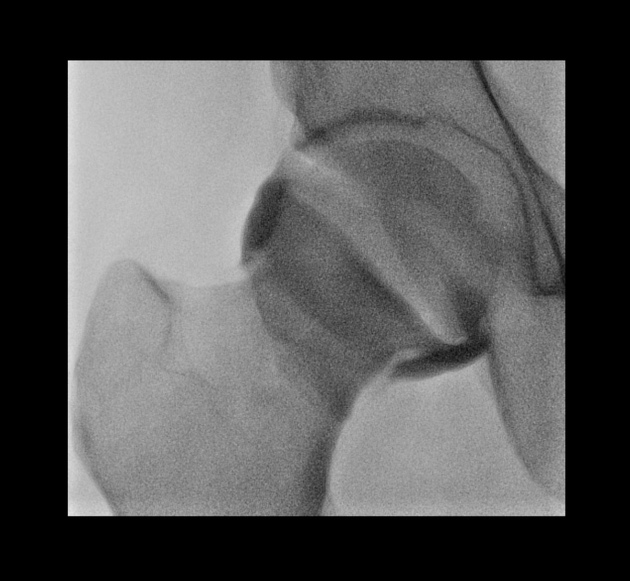
shoulder: instability/labral tears including superior labral anterior posterior (SLAP) tears, humeral avulsion of the glenohumeral ligament (HAGL) injuries, investigation of painful shoulder with normal Xray and MRI.
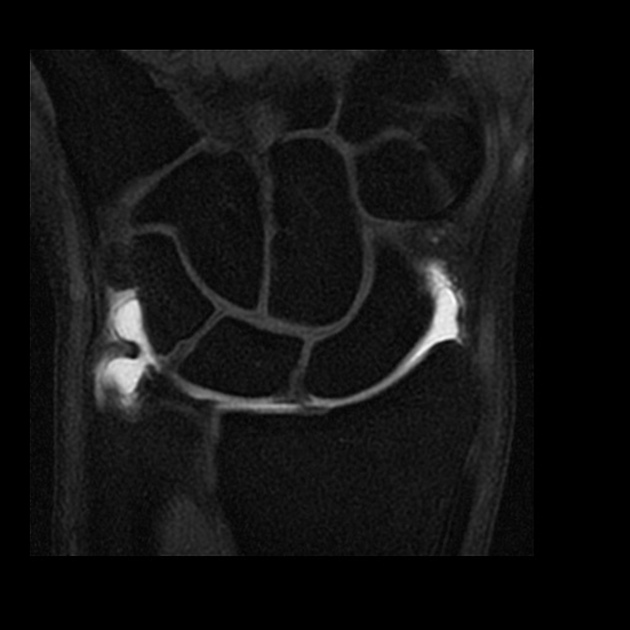
wrist: triangular fibrocartilage (TFC) tear, scapholunate ligament tear
Contraindications
Absolute
anaphylaxis to contrast medium/ injectate
body habitus too large for local MRI
MRI contraindication
Relative
over 50 years of age
unable to remain still for the procedure
Procedure
The arthrogram injection aim is to distend the joint with gadolinium containing solution, but not so distended to cause discomfort 1,2.
Preprocedural evaluation
Relevant imaging should be reviewed and details of the patient confirmed. The patient should have an opportunity to discuss the risks and benefits and consent obtained.
Risks include:
infection
bleeding
allergy
Driving is not advised after any injection, particularly if a local anesthetic is used. The reasons include an inability to perform an emergency procedure and be in safe control of a vehicle.
Technique
Patient positioning and technique will vary depending on the joint, method of access and individual performing the injection 3.
Steps of an arthrogram injection
check for allergies and if on blood thinners
consent
optimize patient positioning
optimize imaging and mark skin
clean skin and draw up appropriate medications
local anesthesia along the proposed needle path
obtain joint access with image guidance
confirm an intra-articular position
administer MR arthrogram injectate
apply dressing/ band-aid
The more commonly performed MR arthrograms are of the shoulder and hip. A glenohumeral joint injection (technique) can either be performed from anterior 1,2,4 or posterior 5 approaches. The hip is injected from an anterior approach 1,2.
Equipment
skin marker and a metal rod for marking (fluoroscopy)
ultrasound machine and sterile probe cover (ultrasound)
skin cleaning product
sterile drape
sterile field and tray for sharps
syringe selection
larger bore drawing up needle/ quill
needle to administer local anesthetic i.e. 25-gauge needle
needle to cannulate the joint i.e. 22-gauge Quincke needle
short extension tubing
injectants i.e. local anesthetic, saline, iodinated contrast, gadolinium
sterile gauze
adhesive dressing
Syringe selection
The injected solutions used in MR arthrogram injections are clear, therefore syringe selection is an important way of identifying the different solutions.
A suggested syringe selection for a fluoroscopic MR arthrogram injection -
5 mL syringe: local anesthetic i.e. 1% lidocaine
10 mL syringe: non-ionic iodinated contrast i.e. iohexol
20 mL syringe: arthrogram injectate
A suggested syringe selection for an ultrasound-guided MR arthrogram injection:
5 mL syringe: local anesthetic i.e. 1% lidocaine
20 mL syringe: arthrogram injectate
Arthrogram injectate
If performing ultrasound-guided injections, an intra-articular position is confirmed with direct visualization, therefore iodinated contrast is not required. Suggested arthrogram injectate mixtures are offered below.
Fluoroscopy:
20mL syringe containing: 0.1 mL gadolinium, 9.9 ml 0.9% saline, 5 mL 0.5% ropivacaine, 5 mL iohexol
Ultrasound-guided:
20mL syringe containing: 0.1 mL gadolinium, 14.9 ml 0.9% saline, 5 mL 0.5% ropivacaine
The dilution of gadolinium is usually 1:200 therefore 0.1mL in 20 mL syringe 1. There are reported chondrotoxic effects of local anesthetics, and intra-articular lidocaine should be avoided. Other lower strength local anesthetics are reported as having less of a chondrotoxic effect. i.e. ropivacaine 6. Some institutions will not use a local anesthetic in their arthrogram injectate mixtures citing the above however its use has been shown to improve comfort and lessen movement artifact 7. Furthermore, a small amount included in the 20 mL arthrogram mixture can be useful diagnostically; if the patient has pain relief post-procedure, the injected joint is likely the pain generator. This combined with the imaging findings can help guide further treatment.
MR arthrogram requests
Request forms will be sent asking for imaging and it is implied a guided injection will take place before cross-sectional imaging. Waiting times are often longer for MR arthrograms and they involve an invasive procedure, therefore stricter guidelines are usually in place. An approximate upper age limit is 50 years old, after which time labral tears and arthropathy are more common. If imaging is requested and indicated in such patients, non-arthrogram MRI imaging is performed initially, and if the non-contrast imaging does not provide a sufficient answer, an MR arthrogram could be considered at that point.
MR arthrogram sequences
Gadolinium and fat are both high signal on T1 weighted sequences, whereas fluid is low signal. By using T1 weighted, fat-saturated sequences in MR arthrograms, we can identify areas that the high T1 signal gadolinium imbibes. Pathology in these areas, such as chondrolabral junction, would be less evident or not appreciable on non-fat saturated and fluid sensitive sequences nor in non-distended joints.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.