Branch retinal artery occlusion (BRAO) refers to the acute obstruction of an arteriolar branch of the central retinal artery, which can lead to retinal ischemia and transient or permanent visual loss. The distribution affecting a branch distinguishes this disease from central retinal artery occlusion, which carries a worse visual prognosis.
On this page:
Epidemiology
Risk factors
Retinal artery occlusions, whether central or branch, are associated with common cardiovascular risk factors 1,7:
- increasing age (older adults)
- cigarette smoking
- hypertension
- hypercholesterolemia
- diabetes mellitus
- carotid artery stenosis
- atrial fibrillation
- cardiac valvular diseases such as aortic stenosis/sclerosis or mitral valve insufficiency
Associations
In turn, symptomatic retinal artery occlusion has an important association with ischemic stroke 1.
Clinical presentation
Patients present with acute onset, painless, monocular visual loss.
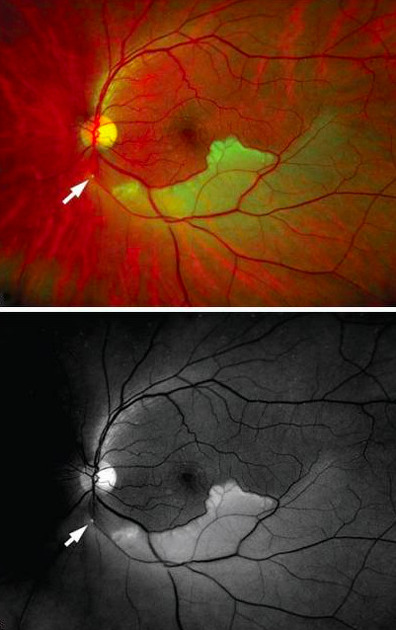
On funduscopic examination, cotton wool spots and retinal whitening occur secondary to retinal ischemia. The findings occur across a sector corresponding to the territory downstream of the branch artery occlusion.
Pathology
Etiology
Most cases of branch retinal artery occlusion are attributed to emboli, which are often directly visualized on ophthalmologic examination 1,2. Unlike with central retinal artery occlusion, giant cell arteritis is not considered a cause of branch retinal artery occlusion except when it is the cilioretinal artery that is involved 8. Non-embolic branch retinal artery occlusion may be related to small vessel disease mechanisms 9. In younger patients, additional considerations include Susac syndrome and hypercoagulable states.
Location
The vast majority of branch retinal artery occlusion involves the temporal branches, most commonly at the proximal bifurcation where the luminal diameter narrows 2.
Radiographic features
Fluorescein angiography
Fluorescein angiography, which visualizes blood flow through the retina following intravenous injection of fluorescein, can show delayed arterial filling in branch retinal artery occlusion 2.
Optical coherence tomography
Optical coherence tomography angiography offers a non-invasive alternative to fluorescein angiography by employing motion contrast imaging for the diagnosis of retinal artery occlusion. In branch retinal artery occlusion, optical coherence tomography angiography shows superficial and deep capillary non-perfusion areas and vessel dilation in areas proximal to artery occlusion 3.
Spectral domain optical coherence tomography shows hyper-reflectivity, increased thickness of inner retinal layers, and decreased reflectivity in the outer retinal layers 4.
Treatment and prognosis
No acute therapies are well proven for symptomatic retinal artery occlusion 1. More than a year following initial presentation for branch retinal artery occlusion, 60% of eyes have a best corrected visual acuity of 20/40 or better 5.
About a quarter of patients with symptomatic branch retinal artery occlusion have concurrent acute cerebral infarction, which is frequently clinically silent 6. These patients are typically referred for urgent evaluation at a stroke center because the near-term risk of stroke is high and some therapies can reduce this risk 1. This evaluation includes blood work as well as imaging of the brain (MRI), carotid arteries (CTA, MRA, or Doppler US), and heart (echocardiography) 10.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.