Bronchopulmonary dysplasia (BPD), particularly affects preterm infants causing significant morbidity and mortality.
On this page:
Terminology
Bronchopulmonary dysplasia and chronic lung disease of prematurity (CLDP) have often been used interchangeably to describe the condition post-treatment of premature infants for respiratory distress syndrome. However, some suggest that there are different underlying pathogeneses and that CLDP encompasses other conditions besides bronchopulmonary dysplasia 12,13.
Various definitions of BPD are used in the literature. A diagnosis of BPD can be made if supplemental oxygen is required at 36 weeks postmenstrual age (PMA). The National Institute of Child Health and Human Development, 2019, used the mode of respiratory support required at 36 weeks PMA, which correlates with the severity of BPD.
Epidemiology
Risk factors
prematurity
intrauterine growth restriction
maternal smoking during pregnancy.14
conventional mechanical ventilation (overdistension)
oxygen toxicity (free radicals)
infection
Pathology
In infants treated with surfactant and steroids, there are fewer, larger alveoli and a smaller surface for gas exchange. The interstitium is thickened and pulmonary vascular development is affected, increasing vascular resistance and causing pulmonary hypertension.
Aetiology
Before the introduction of surfactants and steroids, ventilation and oxygen toxicity led to airway injury, inflammation and fibrosis.
Radiographic features
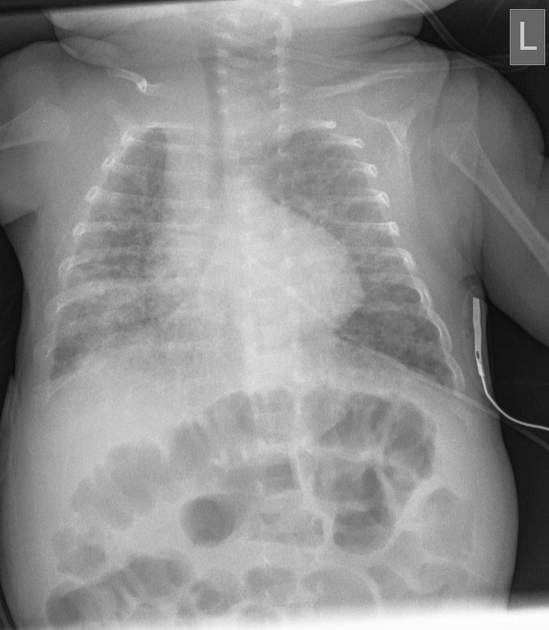
Plain radiograph
ill-defined reticular markings with interspersed rounded lucent areas diffusely involving hyperinflated lungs 1
the lungs may have relatively normal AP diameter on the lateral film
presence of cardiomegaly may indicate the development of pulmonary hypertension
in chronic cases, the lateral film may show a much narrower AP diameter compared with the chest width on the frontal film
-
other described features include of established bronchopulmonary dysplasia include 15
interstitial thickening
areas of atelectasis
Radiographic phases of bronchopulmonary dysplasia
Stage 1: first 3 days - identical to respiratory distress syndrome i.e. generalised granular opacities and reduced lung volumes
Stage 2: 4 to 10 days - bilateral lung whiteout with air bronchograms; heart borders completely obscured by the lung density
Stage 3: 10 to 20 days - small rounded focal radiolucencies distributed throughout both lungs
Stage 4: > 1 month - enlargement of radiolucent areas; hyperinflation and cardiomegaly 17
CT
mosaic lung parenchymal pattern with areas of low attenuation and focal air trapping on expiratory HRCT (considered the most sensitive finding for predicting severity)
bronchial wall thickening (considered the most frequent finding)
small subpleural triangular/linear opacities
Bronchiectatic changes are usually not considered a feature 4.
Treatment and prognosis
Infants who survive neonatal bronchopulmonary dysplasia often show a slow but continuous improvement in respiratory status. Young adult survivors who have had moderate and severe bronchopulmonary dysplasia may have residual functional and characteristic structural pulmonary abnormalities; of these, the most notable is pulmonary emphysema 7.
History and etymology
It is thought to have been first described in 1967 by W Northway et al. 16
Differential diagnosis
General imaging differential considerations include:
pulmonary interstitial emphysema (has an acute course)




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.