Cardiac arrest is the term used for the abrupt loss of cardiac pump function such that an adequate circulation cannot be maintained. Despite recent modest improvements in survival, it usually leads to death, if not immediately treated. Arrests may be in-hospital or out-of-hospital.
On this page:
Epidemiology
The epidemiology of cardiac arrest varies based on whether we are considering in- or out-of-hospital arrests, although at least one large study (from 2020) shows that the previously assumed marked differences in these two groups may be illusory 9.
Worldwide, the incidence of cardiac arrest is not known 1, however, studies in the US have shown that there are almost 300,000 in-hospital arrests per annum 1. Age-wise, cardiac arrests have a mean age of occurrence in the mid-sixties, with a small majority being men (58%) 1. Non-shockable rhythms are much more common, accounting for about 80% of arrests.
Younger adult patients
A retrospective study of over 3,000 young (<35 years) out-of-hospital cardiac arrest patients in London, UK, found that three-quarters were over 18 years old, the majority being male, and cardiac etiology was the commonest underlying cause. Common non-cardiac causes of arrest in young adult males were attempted suicides, especially hanging and overdoses 8.
Pediatric
In infants less than 12-months-old, sudden infant death syndrome (SIDS) was the commonest trigger for cardiac arrest in the large young patient study performed in London, UK 8.
Clinical presentation
Patients may initially be awake, although once the heart stops, loss of consciousness rapidly ensues due to a critical lack of perfusion of the brain.
Cardiac arrest is usually straightforward to recognize, with classic signs and symptoms:
pallor
agonal/absent breathing
absent peripheral pulses
severe hypotension/unmeasurable blood pressure
poor oxygen saturations
unconscious (low GCS)
Pathology
Etiology
Over half of all cardiac arrests are secondary to a cardiac cause, with respiratory deterioration accounting for most of the remainder (up to 40%) 1. Many arrests will be multifactorial.
The so-called reversible causes should always be considered during the acute management of an arrest 1,6,7.
Cardiac
myocardial infarction (MI) usually due to coronary arterial disease
Respiratory
hypoxia (commonest cause)
Neurological
cerebral ischemia/hemorrhage: rare as cause of in-hospital arrest
Others
hypovolemia, usually massive hemorrhage
hypothermia e.g. near drowning, exposure
metabolic e.g. hypo-/hyperkalemia, hypoglycemia, hypocalcemia, severe acidosis
toxins: includes carbon monoxide, opioids, methadone, benzodiazepines
Reversible
The "reversible causes" represent a re-ordering of the causes so far described to ensure that key etiologies are always considered 7.
"4 Hs and 4 Ts"
hypoxia
hypovolemia
hypo-/hyperkalemia, hypoglycemia, hypocalcemia, severe acidosis
thrombosis: pulmonary embolism or acute coronary syndrome
toxins
Types
Cardiac arrest can be subtyped according to whether the presenting arrhythmia can be successfully treated with a shock from a defibrillator or not. The majority of cardiac arrests are with non-shockable rhythms.
-
non-shockable rhythms (80%)
-
shockable rhythms (20%)
Radiographic features
Ultrasound
Point of care ultrasound (PoCUS) has been used to assess cardiac arrest patients in emergency departments.
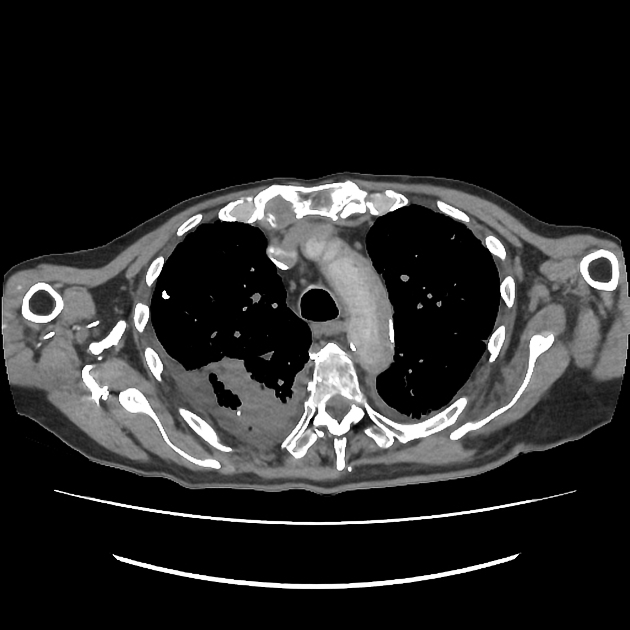
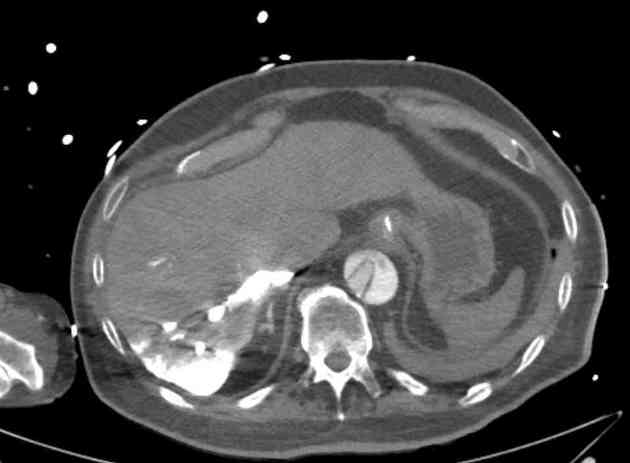
CT
Cardiac arrest is diagnosed clinically however occasionally a patient will be periarrest or have arrested just prior to, or even during, an imaging exam. Several case reports have described the findings on CT in this patient cohort 3,4:
Described CT features include:
absence of contrast media in the pulmonary arteries, aorta and left heart
-
IVC level sign: blood-dependent contrast level in venae cavae due to stasis of contrast media
may be seen in non-arrest scenarios, e.g. hypovolemic shock
Treatment and prognosis
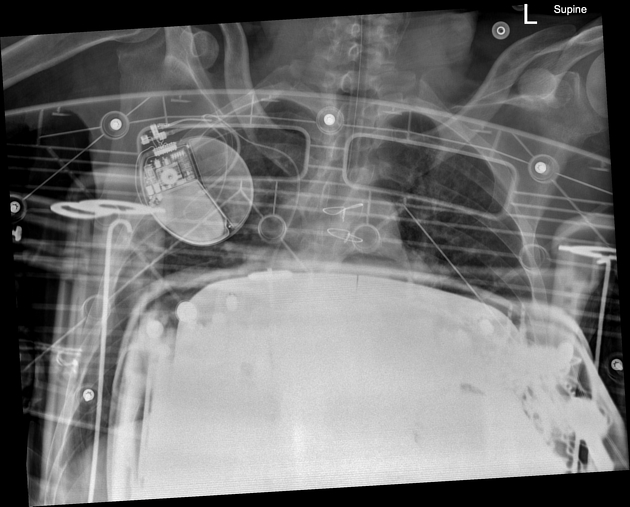
Cardiopulmonary resuscitation (CPR) is the gold standard care performed for all patients in cardiac arrest 1. The algorithms have been modified somewhat over the years as the real-life evidence base has expanded.
Successful CPR results in return of spontaneous circulation (ROSC).
Survival post-arrest remains poor, with a maximal 25% in-hospital cases reaching discharge 2 with the chance of survival outside-hospital being much worse. Nevertheless, long term disability may still be an issue.
Poor prognostic factors for in-hospital arrests from a large meta-analysis 2:
-
pre-arrest
male sex
older age
-
intra-arrest
prolonged resuscitation time
tracheal intubation
However, several conditions were correlated with improved outcomes for in-hospital arrests ref:
witnessed arrest
arrest in a monitored environment
daytime arrest
shockable rhythm
It is also known that shockable rhythms are associated with a better prognosis in the out-of-hospital arrest scenario 2,5.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.