Disclosures
- updated 20 Jan 2023:
Nothing to disclose
Updates to Article Attributes
Cerebellar, hippocampal, and basal nuclei transient oedema with restricted diffusion (CHANTER) syndrome is a recently described constellation of imaging findings in adults with opioid neurotoxicity. It is characterised by cytotoxic oedema in the bilateral hippocampi and cerebellar cortices, and variably in the basal ganglia 1.
This entity likely falls within a pathophysiologic spectrum with paediatric opioid use‐associated neurotoxicity with cerebellar oedema (POUNCE) syndrome (which occurs in children), and opioid-associated amnestic syndrome (which involves the hippocampi alone). It is probably distinct from chasing the dragon leukoencephalopathy, which predominantly affects white matter and occurs after inhalational heroin use.
Clinical presentation
Patients present with a decreased level of consciousness 1,2.
Radiographic features
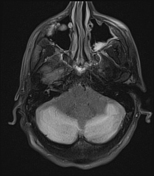
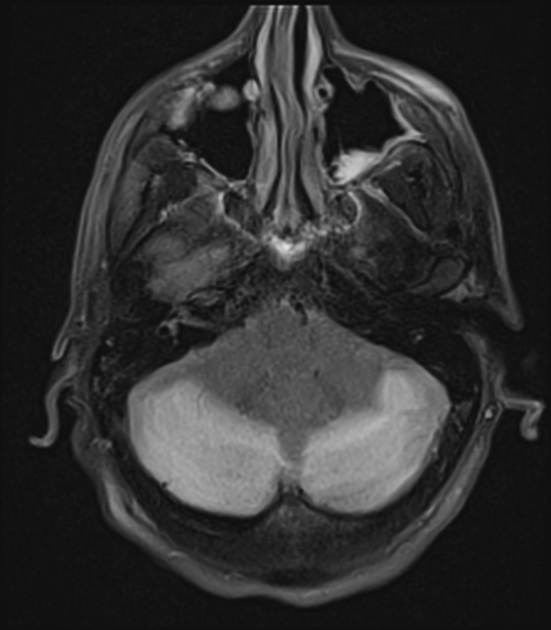
Imaging shows cerebellar oedema, which may progress to cause hydrocephalus 2. MRI demonstrates bilateral, symmetric restricted diffusion in the grey matter of the cerebellum and hippocampi, as well as asymmetric involvement of the basal ganglia 1,2. The cerebral cortex is spared 1.
History and etymology
The syndrome was first described by an American group of clinicians in a seminal case series in 2019 1.
Differential diagnosis
-<p><strong>Cerebellar, hippocampal, and basal nuclei transient oedema with restricted diffusion (CHANTER) syndrome </strong>is a recently described constellation of imaging findings in adults with opioid neurotoxicity. It is characterised by <a href="/articles/cytotoxic-cerebral-oedema">cytotoxic oedema</a> in the bilateral <a href="/articles/hippocampus">hippocampi</a> and <a href="/articles/cerebellum">cerebellar cortices</a>, and variably in the <a href="/articles/basal-ganglia">basal ganglia</a> <sup>1</sup>.</p><p>This entity likely falls within a pathophysiologic spectrum with <a href="/articles/pediatric-opioid-useassociated-neurotoxicity-with-cerebellar-edema-pounce-syndrome">paediatric opioid use‐associated neurotoxicity with cerebellar oedema (POUNCE) syndrome</a> (which occurs in children), and <a href="/articles/opioid-associated-amnestic-syndrome">opioid-associated amnestic syndrome</a> (which involves the hippocampi alone). It is probably distinct from <a href="/articles/heroin-induced-leukoencephalopathy">chasing the dragon leukoencephalopathy</a>, which predominantly affects white matter and occurs after inhalational heroin use.</p><h4>Clinical presentation</h4><p>Patients present with a decreased level of consciousness <sup>1,2</sup>.</p><h4>Radiographic features</h4><p>Imaging shows cerebellar oedema, which may progress to cause hydrocephalus <sup>2</sup>. MRI demonstrates bilateral, symmetric restricted diffusion in the grey matter of the cerebellum and hippocampi, as well as asymmetric involvement of the basal ganglia <sup>1,2</sup>. The cerebral cortex is spared <sup>1</sup>.</p><h4>History and etymology</h4><p>The syndrome was first described by an American group of clinicians in a seminal case series in 2019 <sup>1</sup>.</p><h4>Differential diagnosis</h4><ul>-<li>-<a href="/articles/hypoxic-ischaemic-encephalopathy-adults-and-children">hypoxic-ischaemic encephalopathy</a> can also cause restricted diffusion in the hippocampus, cerebellar cortex, and deep grey nuclei, but cerebral cortex should also be involved</li>-<li><a href="/articles/heroin-induced-leukoencephalopathy">chasing the dragon leukoencephalopathy</a></li>-<li><a href="/articles/posterior-reversible-encephalopathy-syndrome-1">posterior reversible encephalopathy syndrome</a></li>- +<p><strong>Cerebellar, hippocampal, and basal nuclei transient oedema with restricted diffusion (CHANTER) syndrome </strong>is a recently described constellation of imaging findings in adults with opioid neurotoxicity. It is characterised by <a href="/articles/cytotoxic-cerebral-oedema">cytotoxic oedema</a> in the bilateral <a href="/articles/hippocampus">hippocampi</a> and <a href="/articles/cerebellum">cerebellar cortices</a>, and variably in the <a href="/articles/basal-ganglia">basal ganglia</a> <sup>1</sup>.</p><p>This entity likely falls within a pathophysiologic spectrum with <a href="/articles/pediatric-opioid-useassociated-neurotoxicity-with-cerebellar-edema-pounce-syndrome">paediatric opioid use‐associated neurotoxicity with cerebellar oedema (POUNCE) syndrome</a> (which occurs in children), and <a href="/articles/opioid-associated-amnestic-syndrome">opioid-associated amnestic syndrome</a> (which involves the hippocampi alone). It is probably distinct from <a href="/articles/heroin-induced-leukoencephalopathy">chasing the dragon leukoencephalopathy</a>, which predominantly affects white matter and occurs after inhalational heroin use.</p><h4>Clinical presentation</h4><p>Patients present with a decreased level of consciousness <sup>1,2</sup>.</p><h4>Radiographic features</h4><p>Imaging shows cerebellar oedema, which may progress to cause hydrocephalus <sup>2</sup>. MRI demonstrates bilateral, symmetric restricted diffusion in the grey matter of the cerebellum and hippocampi, as well as asymmetric involvement of the basal ganglia <sup>1,2</sup>. The cerebral cortex is spared <sup>1</sup>.</p><h4>History and etymology</h4><p>The syndrome was first described by an American group of clinicians in a seminal case series in 2019 <sup>1</sup>.</p><h4>Differential diagnosis</h4><ul>
- +<li>
- +<a href="/articles/hypoxic-ischaemic-encephalopathy-adults-and-children">hypoxic-ischaemic encephalopathy</a> can also cause restricted diffusion in the hippocampus, cerebellar cortex, and deep grey nuclei, but cerebral cortex should also be involved</li>
- +<li><a href="/articles/heroin-induced-leukoencephalopathy">chasing the dragon leukoencephalopathy</a></li>
- +<li><a href="/articles/posterior-reversible-encephalopathy-syndrome-1">posterior reversible encephalopathy syndrome</a></li>
Image
2
MRI (FLAIR)
(
create
)





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.