Choroidal haemangiomas are benign vascular hamartomatous tumours of the choroid.
They present in two forms based on the extent of choroidal involvement:
circumscribed choroidal haemangioma (CCH): solitary tumour with no systemic associations
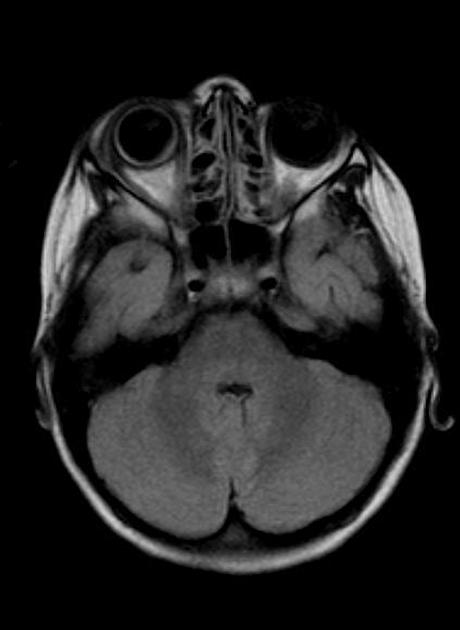
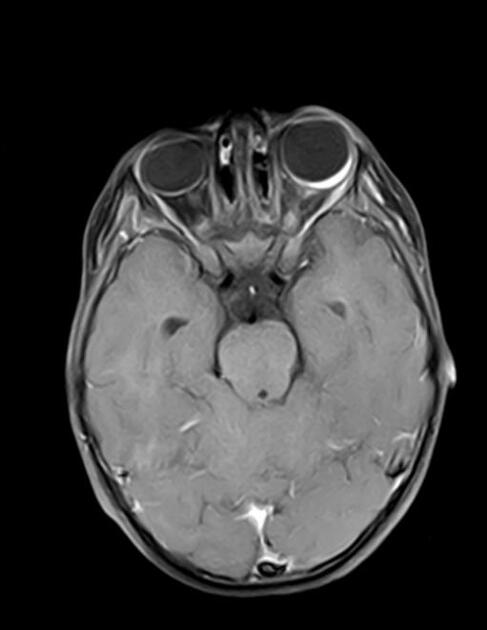
diffuse choroidal haemangioma (DCH): usually in association with Sturge-Weber syndrome
On this page:
Epidemiology
The exact incidence worldwide is not known but it is rare. 200 diagnoses of circumscribed choroidal haemangioma made from 1974-2000 in Wills Eye Institute. Approximately half of patients with Sturge-Weber syndrome have diffuse choroidal haemangioma. Nearly all reported cases are in Caucasians and there is no gender preference.
Clinical presentation
Mostly asymptomatic and incidentally diagnosed with routine ophthalmic examinations:
circumscribed choroidal haemangioma presents with symptoms in 3rd-6th decades of life
diffuse choroidal haemangioma presents with symptoms in 1st-2nd decades of life
Patients also may present with metamorphopsia and reduced visual acuity. Choroidal haemangiomas can also present with leukocoria.
Pathology
No known genetic predisposition for circumscribed choroidal haemangioma. Sturge-Weber syndrome is entirely sporadic and is associated with diffuse choroidal haemangioma.
Radiographic features
Angiography
fundus fluorescein angiography (FFA): hyper-fluorescence in pre-arterial or early arterial phase, followed by late staining and leakage
indocyanine green angiography (ICGA): early intense hyper-fluorescence followed by dye washout in late frames (tumour hypo-fluorescence with rim of hyper-fluorescence)
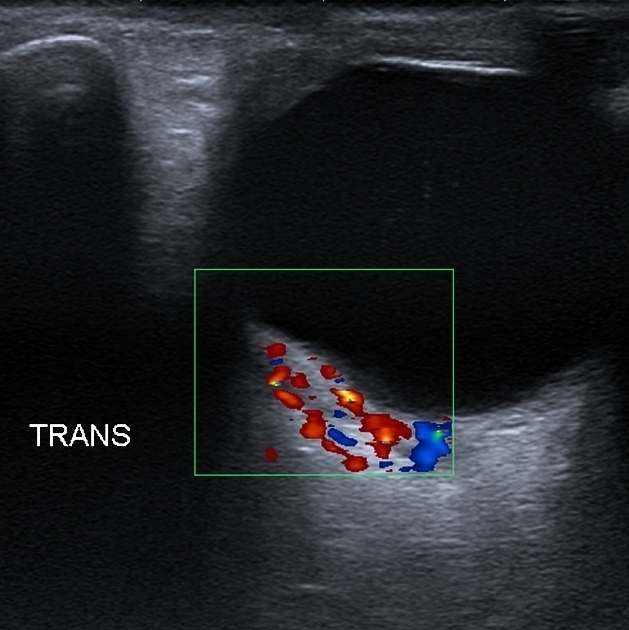
Ultrasound
A-scan: high internal reflectivity
B-scan: acoustic features similar to adjacent (normal) choroid. Choroidal thickening, especially in diffuse choroidal haemangioma
Optical coherence tomography
detection of retinal changes such as fluid changes, underlying geographical atrophy etc
useful to evaluate treatment response and long-term monitoring
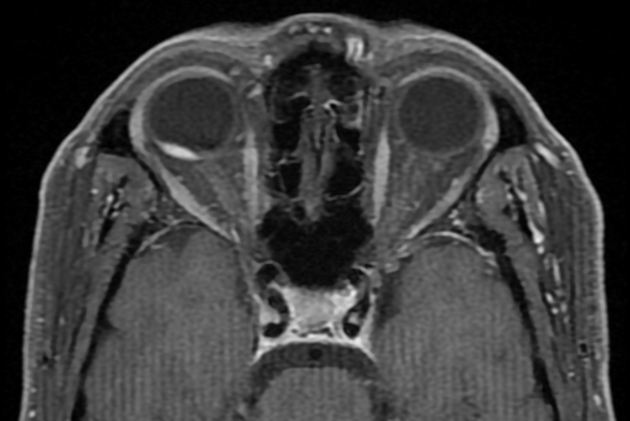
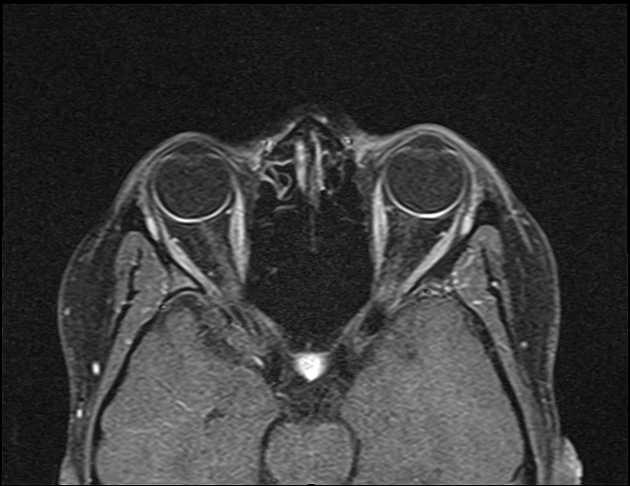
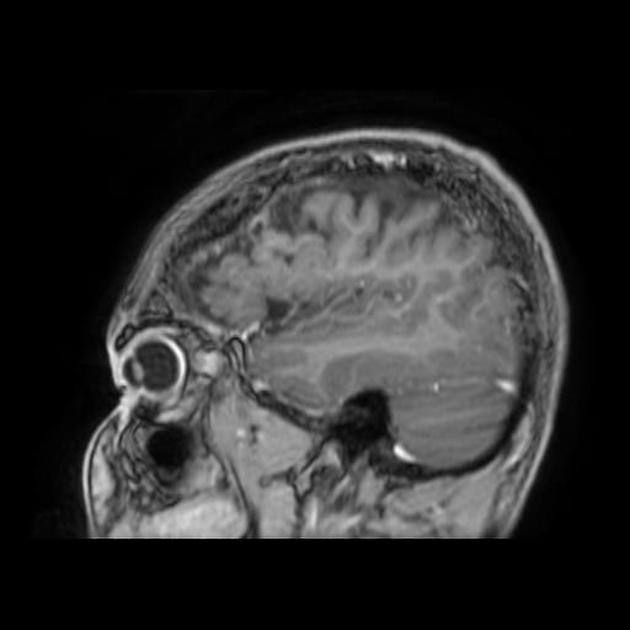
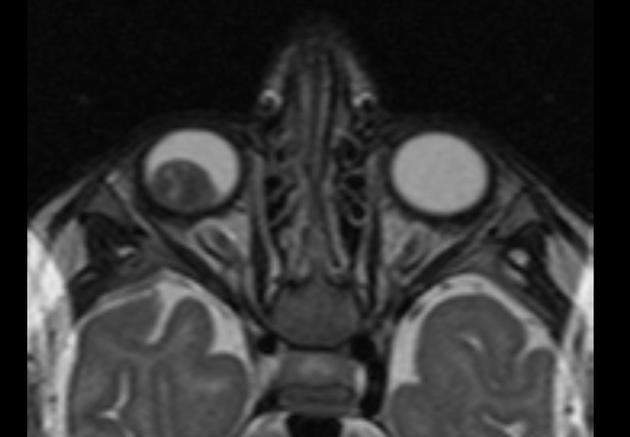
MRI
T1: hyperintense compared to the vitreous
T1 C+ (Gd): show marked enhancement
T2: hyperintense or isointense compared to the vitreous
Treatment and prognosis
Observation if asymptomatic. Diffuse choroidal haemangioma need to be worked up for Sturge-Weber syndrome and managed accordingly. The end-point of treatment is resolution of fluid and not complete regression of tumour:
photodynamic therapy (PDT) with verteporfin is the treatment of choice for CCH and has been used successfully for treatment of diffuse choroidal haemangioma
plaque radiotherapy: second-line therapy failing PDT, or unsuitable for PDT
laser photocoagulation: use limited to extrafoveal circumscribed choroidal haemangiomas when PDT not possible; high rates of recurrent subretinal fluid despite initial success
external beam radiotherapy: commonly used for management of diffuse choroidal haemangioma
Prognosis for circumscribed choroidal haemangioma generally improving with PDT, however, very much dependent on the location of the lesion. A long delay between the onset of symptoms and treatment is associated with poorer visual outcome.
Complications include neovascular glaucoma secondary to chronic extensive retinal detachments, with some requiring enucleation.
Differential diagnosis
amelanotic choroidal melanoma is hyperintense on T1WI, hypointense on T2WI
central serous chorioretinopathy
inflammatory conditions
Practical points
prompt referral to specialist ophthalmology care
always remind patients to report any new symptoms such as increased metamorphopsia, reduced visual acuity, photopsia or visual field defects
PDT is the treatment of choice for circumscribed choroidal haemangioma, but asymptomatic patients can be observed without treatment
circumscribed choroidal haemangioma should be considered in the differential diagnosis of patients diagnosed with central serous chorioretinopathy





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.