Cubital tunnel syndrome is an ulnar nerve compression neuropathy (tunnel syndrome) due to pathological compression of the ulnar nerve at the elbow proximal, within, and distal to the cubital tunnel 12.
On this page:
Epidemiology
The compression of the ulnar nerve at the elbow is the second most common peripheral neuropathy of the upper extremity after carpal tunnel syndrome, with an incidence of ~3% (range 1.9 to 5.8%) 1,3,12.
Diagnosis
Diagnosis depends on the combination of history and clinical examination, and investigations, such as electromyography, ultrasound, and MRI, are useful tools, but there are no defined diagnostic criteria/pathways 12,13.
Clinical presentation
Ulnar nerve compression can result in altered sensation in the little and ring fingers. In many patients, sensory loss is often the first symptom to be reported 12. As the condition progresses, there may be hand clumsiness, in particular, with a weak thumb and grip strength 12, as the ulnar nerve is the principal motor supply to the intrinsic muscles of the hand. In well‐established cases, there may be marked wasting of the small muscles of the hand and the ulnar‐sided muscles of the forearm 4.
Pathology
The ulnar nerve is vulnerable to stretching and compression injury as it crosses the elbow joint, which undergoes a large arc of flexion during normal range of motion. The cubital tunnel represents one of several small passages through which the ulnar nerve passes near the elbow and is considered the most common specific site of injury 1.
During normal elbow flexion, the ulnar nerve experiences tension and axial compression due to increased pressure within the cubital tunnel, up to twenty-fold 1. Any local structural abnormality may exacerbate the mechanical forces on the nerve, which may result in neuropathy.
Other potential points of compression besides the cubital tunnel include the arcade of Struthers, against the medial humeral epicondyle just proximal to the cubital tunnel, and between the humeral and ulnar heads of the flexor carpi ulnaris distal to the cubital tunnel.
Etiology
Specific causes of ulnar neuropathy at the cubital tunnel include:
-
intrinsic causes
neural mass, e.g. peripheral nerve sheath tumor, traumatic neuroma, intraneural ganglion cyst 12
subluxation/dislocation of the ulnar nerve from congenital laxity in fibrous tissue 12
-
extrinsic compression
anconeus epitrochlearis muscle: most common structural cause 12
bone/joint-related pathology, e.g. humeral fracture, osteophytes/enthesophytes, synovitis, chondromatosis 12
osteophytic bony spur arising from the epicondyle or olecranon
soft-tissue mass/tumor, e.g. ganglion, osteochondroma, hematoma 12
thickened cubital tunnel retinaculum or arcuate ligament of the flexor carpi ulnaris muscle 12
post-surgical fibrosis after cubital tunnel release 12
Radiographic features
Exact imaging features may vary dependent on the underlying cause. Ulnar nerve thickening can be a commonly observed feature.
Plain radiograph
Osseous spurring within the ulnar groove 12 can be seen in patients with chronic nerve irritation due to overuse or posteromedial elbow impingement.
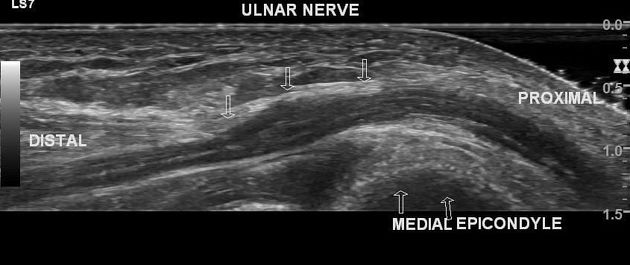
Ultrasound
Ulnar nerve thickening and edematous changes (e.g. hypoechoic, enlarged, loss of fasicular pattern) are findings suggestive of ulnar neuropathy.
Abnormal thickening by measuring the cross-sectional area (CSA) considered as:
>10 mm2 at the level of the medial epicondyle 9,12
>15 mm2 in the cubital tunnel 12
Other suggestive features according to additional studies include:
a ratio of 1.4-1.5:1, comparing the ulnar nerve area at the level of the cubital tunnel with that proximal to the cubital tunnel 9,12
>2 mm2 CSA between sides
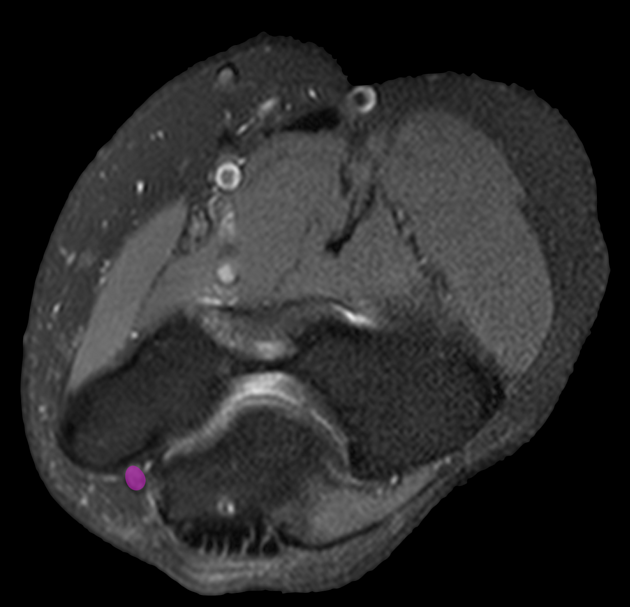
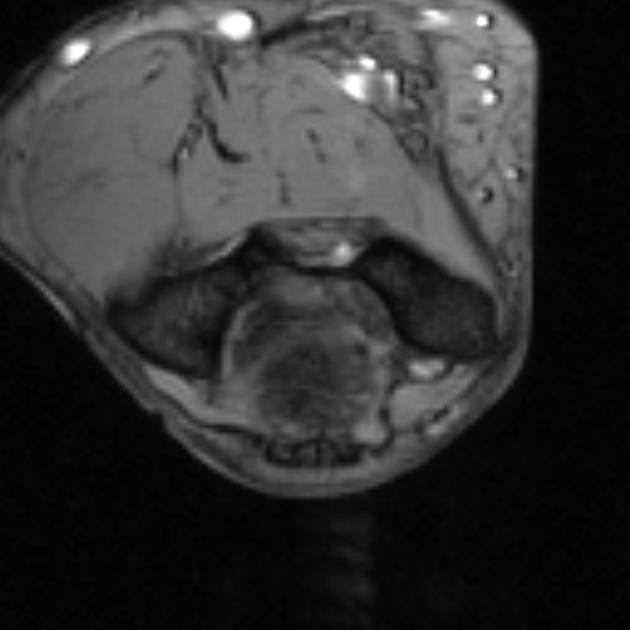
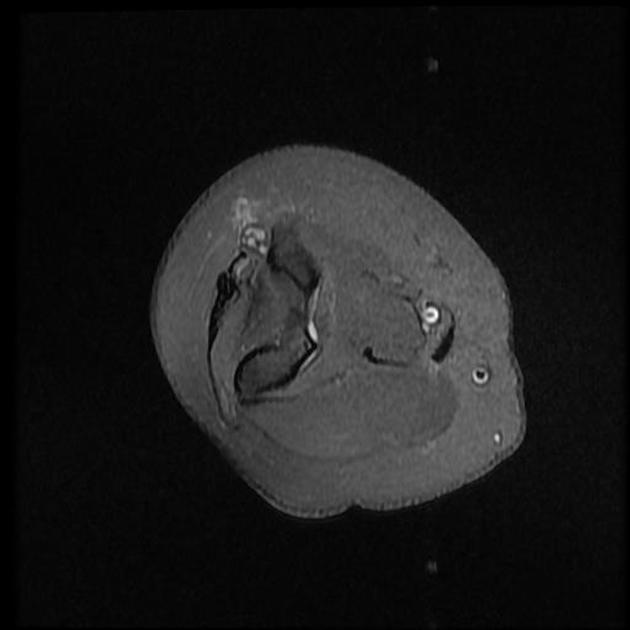
MRI
Accurate assessment for ulnar neuropathy on MRI can be challenging, as the primary imaging features (nerve thickening, increased T2 intensity) may be present in asymptomatic cases. The following findings within the cubital tunnel are suggestive of ulnar neuropathy:
-
ulnar nerve thickening
>11 mm2 in cross-sectional area and an abnormal-to-normal CSA ratio of 1.5 12
-
ulnar nerve T2 hyperintensity
independently, this is non-specific and seen in up to 60% of asymptomatic elbows 12
the degree of hyperintensity may be relatively higher in clinically-significant ulnar neuropathy 7
loss of normal fascicular pattern 12
edema-like signal changes or atrophy of the flexor carpi ulnaris and flexor digitorum profundus muscles may be seen secondary to ulnar neuropathy 12
Differential diagnosis
Ulnar neuropathy near the elbow may result from compression at three other sites, which may require a different type of treatment:
arcade of Struthers: a variable fascial thickening along the medial distal arm overlying the ulnar nerve
posterior to medial humeral epicondyle (just proximal to the cubital tunnel)
between the ulnar and humeral heads of flexor carpi ulnaris (just distal to the cubital tunnel)
Alternatively, the ulnar nerve may be injured at the elbow from repetitive ulnar nerve subluxation/dislocation during resisted elbow extension, e.g. bench press or pitching 1. This may present with a medial elbow "snapping" sensation (although the snapping may actually represent associated myotendinous subluxation rather than nerve motion). The resulting friction neuropathy may cause similar presentation as cubital tunnel syndrome.
dynamic ultrasound imaging may demonstrate ulnar nerve subluxation/dislocation across the medial humeral epicondyle in real-time







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.