Dermatomyositis is an idiopathic inflammatory myopathy, presumably autoimmune in aetiology, which carries an increased risk of malignancy. It is considered a distinct condition to anti-synthetase syndrome.
On this page:
Epidemiology
There is a recognised female predilection. It has a bimodal age of presentation depending on the variant:
juvenile dermatomyositis (JDM): affects children and tends to be more severe
adult dermatomyositis (ADM): typically affects adults around the age of 50 years
Associations
interstitial lung disease 2: typically gives a patchy and subpleural consolidation with parenchymal bands
malignancy 1: can occur as part of a paraneoplastic syndrome (e.g. lung cancer)
Clinical presentation
The classic presentation is that of a myalgic symmetrical proximal myopathy with associated dermatological changes which includes a dusky-red rash over the face (e.g. heliotrope rash), arms, hands (e.g. Gottron papules), legs (e.g. holster sign) and other features (e.g. V sign and shawl sign) 10. Dysphagia, myalgia, fever and weight loss are other features 7.
Complications
Malignancy
There is a sixfold increased risk of malignancy in dermatomyositis (cf. twofold in polymyositis) 8. Multiple risk factors for the development of malignancy have been identified 8:
>60 years old
male
necrosis of the skin
cutaneous vasculitis
accelerated onset of disease
increased creatine kinase (CK) levels
increased ESR and C-reactive protein (CRP) levels
certain antibodies in adult-onset disease: anti-TIF1γ, anti-NXP2 11
Pathology
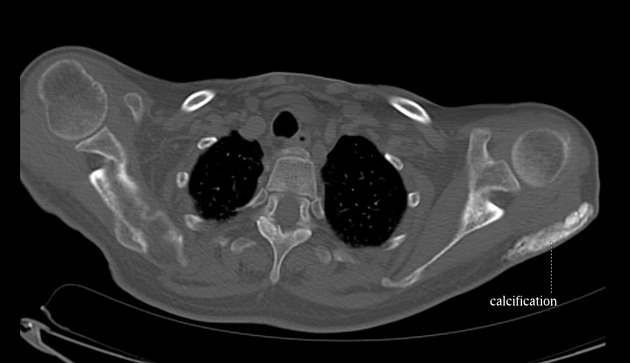
There is cell-mediated injury targeted at striated muscle with resultant atrophy, oedema, coagulation necrosis, fibrosis and calcification. Additionally, it is thought that enhanced type 1 interferon signalling plays a critical role in its pathogenesis 12.
Markers
elevated muscle enzymes (e.g. CK)
-
elevated myositis-specific antibodies
anti-Mi2
anti-MDA5
anti-TIF1γ
anti-NXP2
anti-SAE
Subtypes
Radiographic features
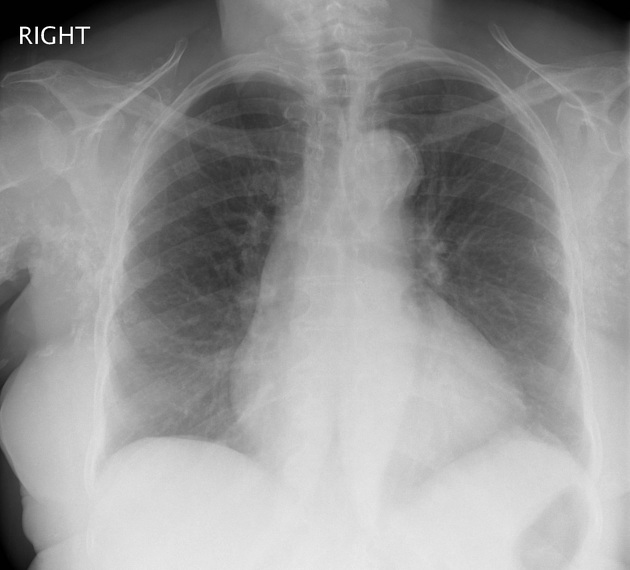
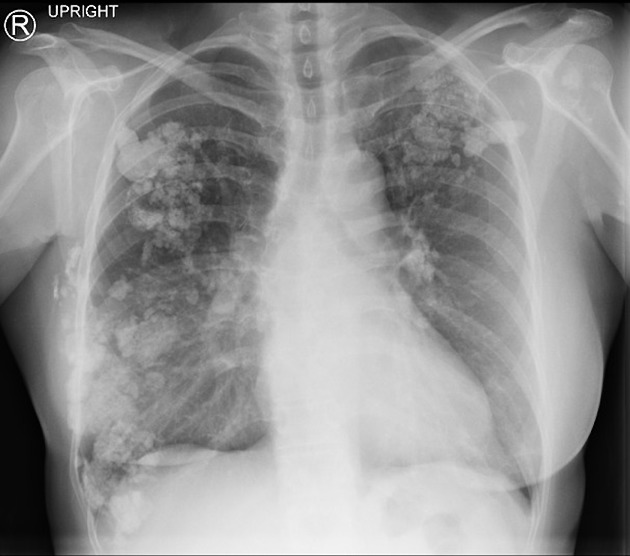
Plain radiograph
-
typically shows dystrophic calcification in muscles and soft tissues (calcinosis universalis)
sheet-like although at least four patterns have been described with childhood dermatomyositis 4
classically seen affecting the thigh regions
chest radiograph may show diaphragmatic elevation
Fluoroscopy
Barium swallow
may show disordered peristalsis involving the upper oesophagus i.e. the portion supplied by skeletal muscle
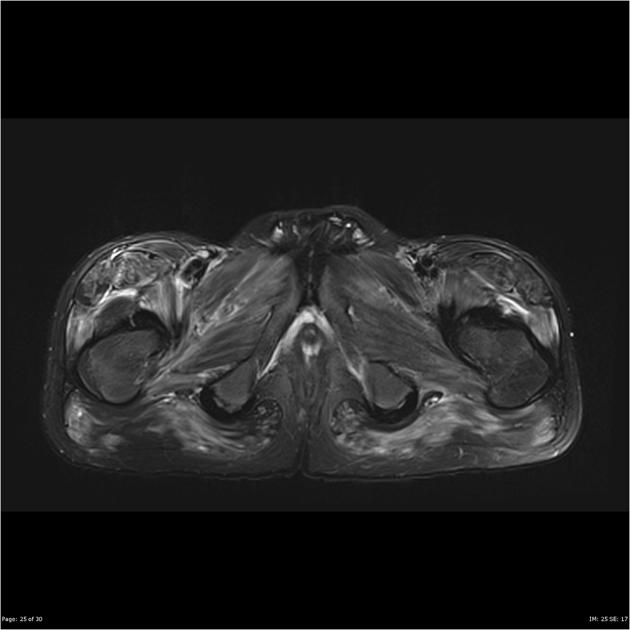
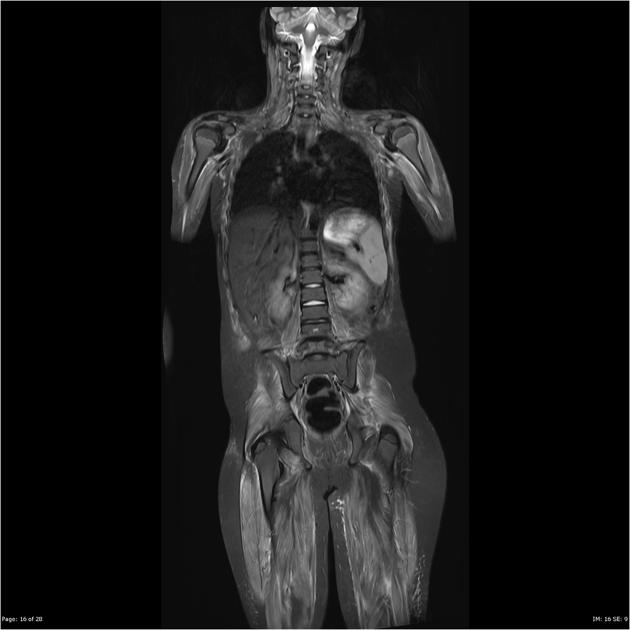
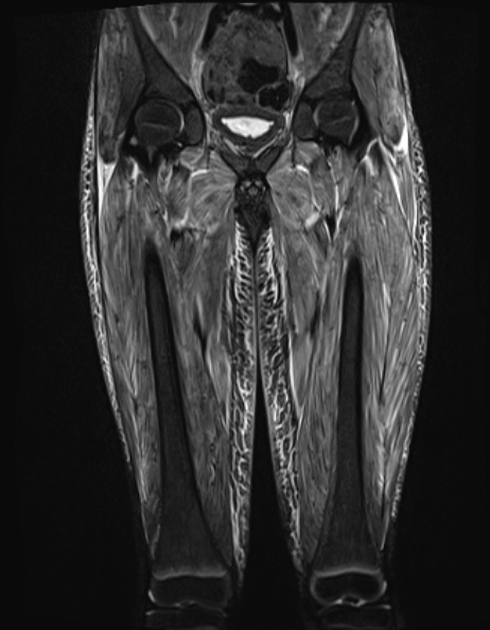
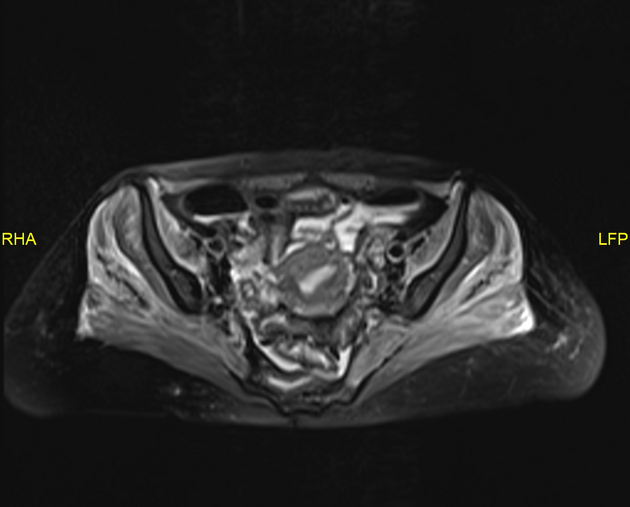
MRI
T2: generally hyperintense signal throughout the affected muscles; calcific areas may be low signal; peri-muscular oedema may additionally appear as high signal; signal intensity may return to normal after treatment 4
Treatment and prognosis
Management of myositis is primarily with immunosuppression. Options include corticosteroids and steroid-sparing agents (e.g. azathioprine, mycophenolate, methotrexate, etc.) 9.
Differential diagnosis
General imaging differential considerations include:
polymyositis: does not affect the skin
Practical points
MRI T2-weighted sequences are useful to guide muscle biopsy:
areas of oedema related to the active inflammatory process
non-specific end-stage fatty atrophic muscle should be avoided
Further imaging in the form of a contrast-enhanced CT of the chest, abdomen and pelvis may be undertaken to exclude an associated primary malignancy.










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.