Diffuse tenosynovial giant cell tumor, previously known as pigmented villonodular synovitis (PVNS), is an uncommon benign condition. It is most commonly monoarticular (~70% in the knee joint), but can occasionally be polyarticular.
Please see the overview article tenosynovial giant cell tumor for content common to both the localized type and diffuse type.
On this page:
Epidemiology
Diffuse tenosynovial giant tumors occur predominantly in early middle age (<40 years) 1,2,11. In intra-articular disease, there is no gender predilection, whereas extra-articular disease has a slight female predominance ref.
Clinical presentation
Presentation usually involves joint swelling, pain and reduced range of motion 11. Hemarthrosis is common 11. Symptoms are usually present for many months or years before the diagnosis is made.
Although unusual in the pediatric population, it is sometimes seen and is more frequently polyarticular. It has also been described in association with 2:
extremity lymphedema
vascular lesions
Pathology
Location
Typically, diffuse tenosynovial giant cell tumors are monoarticular and joints with large synovial surfaces are predictably most frequently affected with the knee being the most frequently affected (~75%) followed by the hip (~10%), ankle, shoulder, elbow, facet joints, and rarely other joints (e.g. temporomandibular joint) 2,6,11.
Macroscopic appearance
Macroscopically, diffuse tenosynovial giant cell tumors are large (>5 cm) and are firm and sponge-like. When intra-articular, a villous pattern is usually present, and when extra-articular there are multiple nodular projections. Their color is typically dark brown and heterogeneous with areas of yellow discolouration (xanthoma cells) 11.
Microscopic appearance
See main tenosynovial giant cell tumor article.
Radiographic features
Plain radiograph
On radiographs, features are relatively non-specific with appearances mainly being those of a joint effusion. Bone density and joint space are preserved until the late stages. No calcification is seen. Extrinsic marginal pressure erosions may be present. There may be suggestion of focal areas of soft tissue swelling surrounding the joint +/- dense soft tissues from hemosiderin deposition.
CT
Joint effusions commonly coexist. The hypertrophic synovium appears as a soft tissue mass, which on account of hemosiderin, may appear slightly hyperdense compared to adjacent muscle. Calcification is very rare in the synovial mass (cf. synovial sarcoma where it is common). Erosions are often well seen on CT.
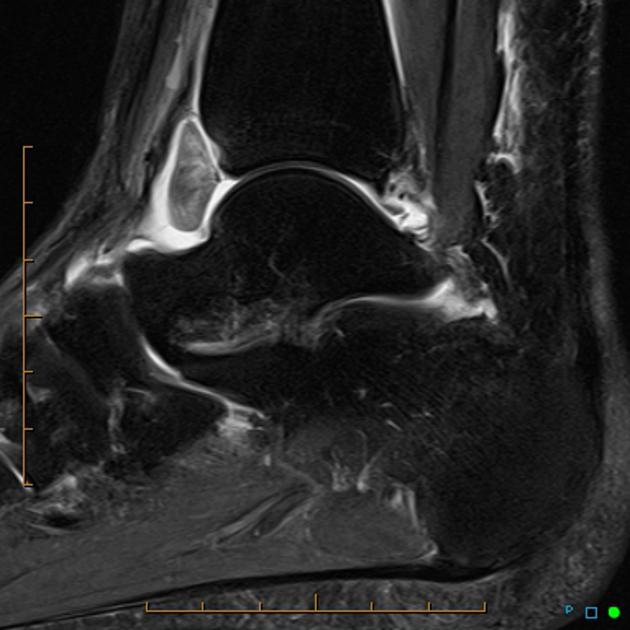
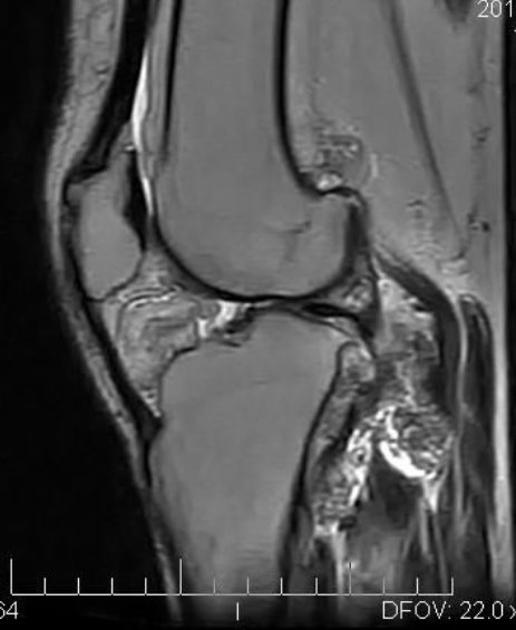
MRI
Typical finding on MRI is extensive synovial proliferation, which may be mass-like, with lobulated or ill-defined margins along with low T1/T2 signal foci due to hemosiderin deposition and/or joint erosions 13.
T2/STIR signal is variable/heterogeneous due to differing amounts of hemosiderin, fat, fluid, fibrous and cellular elements 14.
Signal characteristics
T1: low to intermediate signal
-
T2
variable and heterogeneous
low to intermediate signal
high signal areas may be present, likely due to joint fluid or inflamed synovium
STIR: variable and heterogeneous
GRE: low and may demonstrate blooming artifact
T1 C+ (Gd): variable enhancement
Treatment and prognosis
Treatment is with complete synovectomy, which offers a good prospect of cure, provided all the synovium is excised. This can be difficult and therefore adjuvant treatment is often employed, especially external beam radiotherapy which offers excellent control. Intra-articular injection of yttrium-90 is an alternative 12. Recurrence rates are reported to be ~35% (range 7-60%) 2,11.
Differential diagnosis
The differentials include 15:
synovial osteochondromatosis (calcifications, no blooming on gradient echo unless there is intra-articular hemorrhage)
synovial hemangioma (isointense to skeletal muscle on T1w, calcified phleboliths on radiographs)
synovial sarcoma (aggressive features with direct bone invasion, more often with paraarticular origin)
tendon sheath fibroma (no blooming on gradient echo)
undifferentiated pleomorphic sarcoma (aggressive and destructive lesion with or without calcifications)




















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.