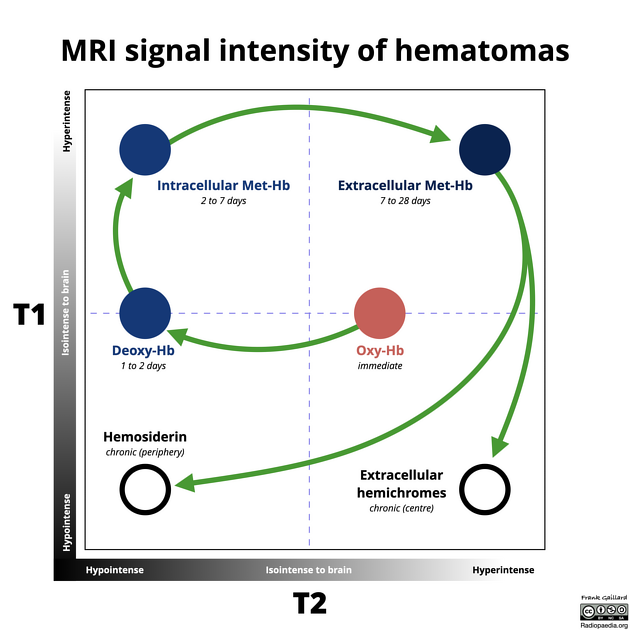
Haemorrhage on MRI has highly variable imaging characteristics that depend on:
the age of the blood
the type of haemoglobin present: oxy-, deoxy- or met-
whether or not the red blood cell walls are intact: i.e. intra- vs extracellular
the MRI sequence
Although MRI is often regarded as being insensitive to acute haemorrhage, this is untrue, particularly with more modern sequences 5,7. However, the appearance of haemorrhage will be different at different times and is not perfectly stereotyped. Caution should therefore be exercised when precisely ageing haemorrhages.
On this page:
Physiology
The oxygenation state of haemoglobin and its location (whether it is contained within red blood cells or diffused in the extracellular space) has a tremendous effect on the imaging effects of blood. The three haemoglobin states to be considered are oxyhaemoglobin, deoxyhaemoglobin and methaemoglobin.
Oxyhaemoglobin accounts for 95% of haemoglobin in arterial blood and 70% in venous blood. It is only weakly diamagnetic, having little T2* effect and only mildly shortening T1 relaxation time 2,6. This is the result of the haem iron existing in its ferrous form (Fe2+) with no unpaired electrons 2.
Deoxyhaemoglobin, in contrast, having lost its oxygen, has four unpaired electrons and is therefore strongly paramagnetic. This results in a substantial signal loss and blooming artifact on T2* weighted sequences such as susceptibility-weighted imaging 2.
Methaemoglobin results from oxidative denaturation of the haem molecule to the ferric (Fe3+) form. It has five unpaired electrons and is also strongly paramagnetic 2.
T1 weighted sequences
Oxyhaemoglobin and deoxyhaemoglobin produce little effect on the T1 signal. The presence of blood proteins results in intermediate T1 signals in hyperacute and acute haemorrhages.
T2* weighted sequences
T2* weighted sequences, such as susceptibility-weighted imaging and gradient-echo are primarily affected by the haemoglobin oxygenation state and whether or not cell lysis has occurred 2.
While contained within red blood cells, resulting in uneven distribution of paramagnetic effects, both deoxyhaemoglobin and methaemoglobin result in signal loss. Once the cells lyse and methaemoglobin is distributed evenly throughout the clot, the local magnetic field distortion is also lost and T2 signal loss fades 2.
Eventually, haemosiderin and ferritin (both strongly paramagnetic) are ingested by monocytes and macrophages andresults once more in unevenly distributed paramagnetic effects and signal loss 2.
Diffusion-weighted imaging
Apparent diffusion coefficient (ADC) maps demonstrate fairly stable values substantially lower than normal white matter in all stages except for chronic (see below), whereas isotropic/trace DWI images, due to the combination of T2 and diffusion effects, demonstrate high-signal-only on hyperacute and late subacute phases 8.
Stages
In general, five stages of haematoma evolution are recognised 8:
-
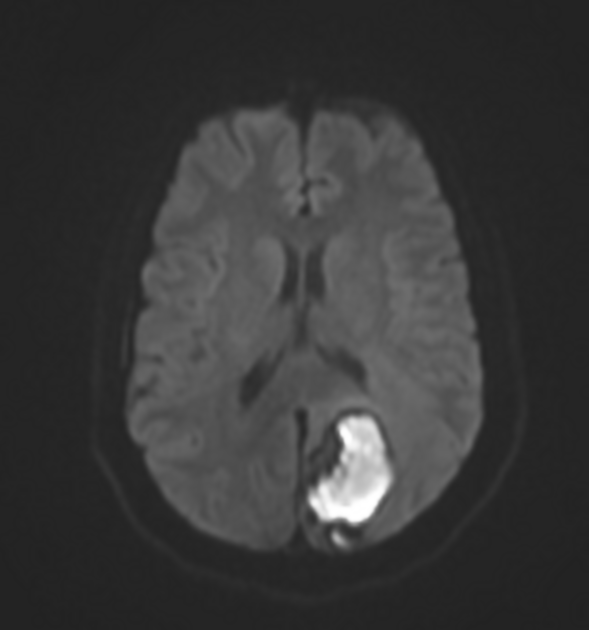
hyperacute (<1 day)
intracellular oxyhaemoglobin
T1: isointense
T2: isointense to hyperintense
DWI: high
ADC: low
SWI: hyperintense, with thin hypointense rim
-
acute (1 to 3 days)
intracellular deoxyhaemoglobin
T1: remains isointense to hypointense
T2: signal intensity drops (T2 shortening) to become hypointense
DWI: low
ADC: low
SWI: hypointense
-
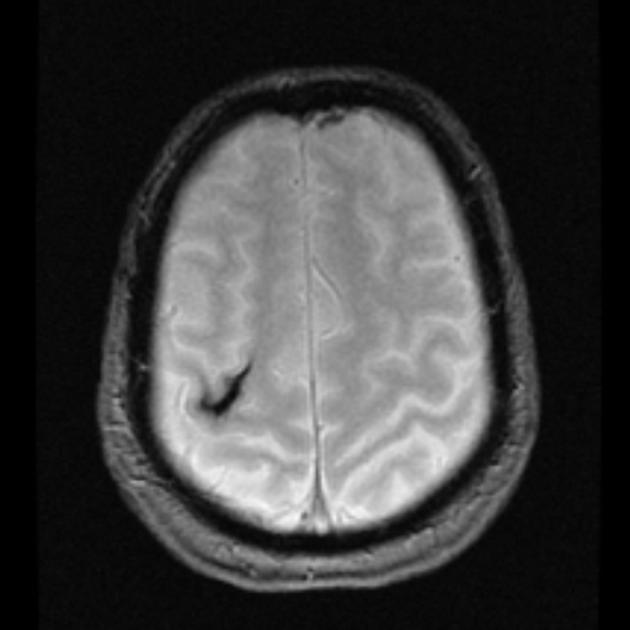
early subacute (3 to 7 days)
intracellular methaemoglobin
T1: signal gradually increases (T1 shortening) to become hyperintense
T2: remains hypointense
DWI: low
ADC: low
SWI: hypointense
-
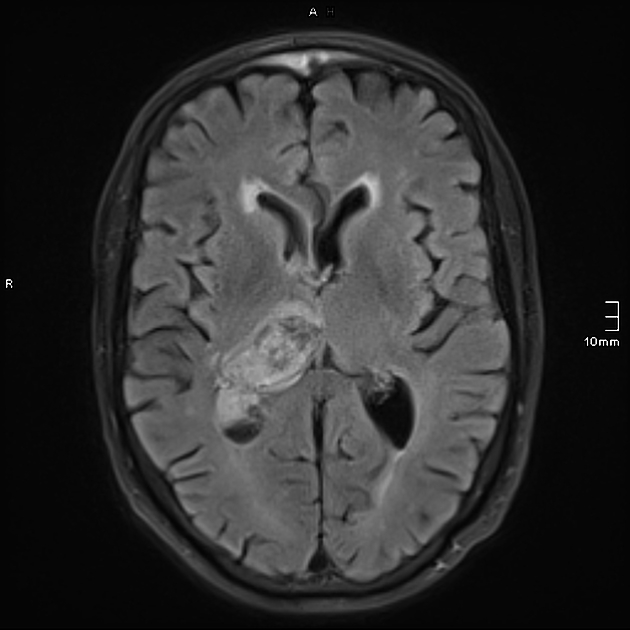
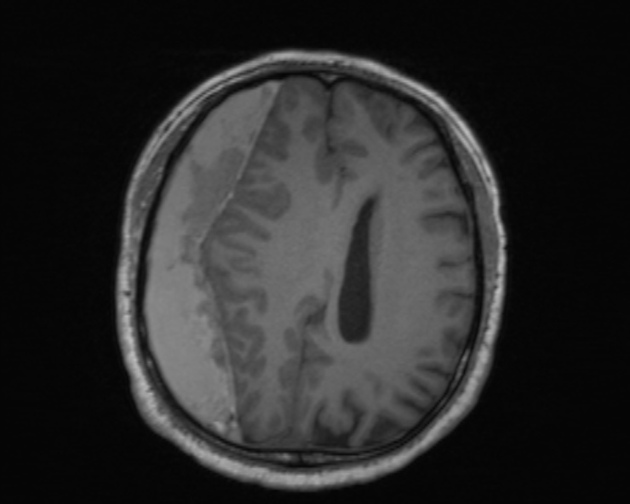
late subacute (7 to 14-28 days)
extracellular methaemoglobin
T1: remains hyperintense
T2: signal gradually increases over the next few weeks as cells break down and extracellular methaemoglobin increases
DWI: high
ADC: low
SWI: hyperintense, with thin hypointense rim
-
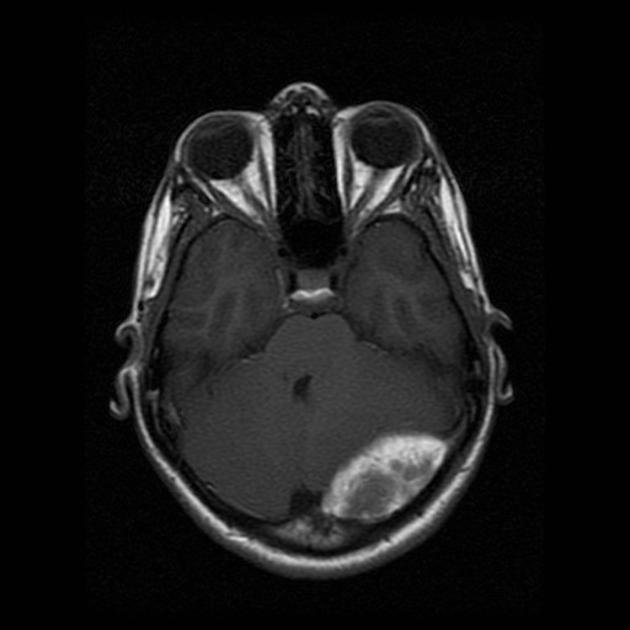
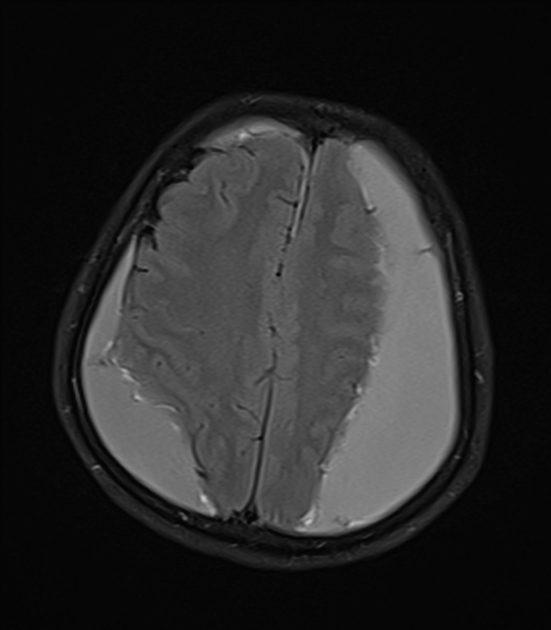
chronic (>14-28 days)
-
periphery
intracellular haemosiderin
T1: hypointense
T2: hypointense
SWI: hypointense rim
-
centre
extracellular hemichromes
T1: isointense
T2: hyperintense
DWI: low
ADC: high
SWI: variable
-
Remembering these may be facilitated by the ageing blood on MRI mnemonics.
Practical points
extracranial blood products age differently from intracranial blood products, and extracranial haematomas often have a heterogeneous appearance, confounding attempts at reliably dating the age of an extracranial haemorrhage 3,4
subacute and chronic blood appears hypointense and blooms on MRI T2* weighted sequences (e.g. susceptibility weighted imaging (SWI))
the presence of blood products in a cavity will result in low ADC values and therefore make the utility of diffusion restriction in diagnosing pus in an abscess useless







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.