Intestinal malrotation is a congenital anatomical anomaly that results from an abnormal rotation of the gut as it returns to the abdominal cavity during embryogenesis. The mesenteric attachment is shortened predisposing to midgut volvulus, and Ladd bands predispose to internal hernia, both potentially fatal.
On this page:
Terminology
In incomplete rotation, the midgut does not rotate more than 180°, thus the cephalad (prearterial proximal) portion of the midgut is fixed to the right of the superior mesenteric artery (SMA) while the caudad (postarterial distal) midgut is fixed directly anterior to the SMA.
In intestinal nonrotation, the midgut does not rotate more than 90°, thus the cephalad midgut is fixed to the right of SMA and the caudad midgut is fixed to the left of SMA. The cephalad midgut will give rise to the small intestine while the caudad midgut will give rise to the cecum and large intestine 13.
Epidemiology
Intestinal malrotation is a congenital abnormality seen in up to 1:500 live births 7.
Associations
It is frequently (~50%) associated with other abdominal anomalies, some of which are causative and others merely associated 5:
-
gastrointestinal tract malformations
gastroschisis and omphalocele: always associated with a degree of malrotation
-
biliary system malformations 11
agenesis of the gallbladder
intra- and extra-hepatic biliary atresia
-
pancreatic malformation 11
hypoplasia or agenesis of the dorsal pancreas
heterotaxy: 70% of individuals will have a malrotation
hypospadias 11
Diagnosis
Imaging demonstrates the abnormal positioning of the bowel, related abnormalities and complications.
Clinical presentation
The clinical presentation of malrotation often correlates with the age of onset 5.
In the infant, the most common presentation is with midgut volvulus. Patients with intestinal nonrotation have a lower incidence of midgut volvulus than other types of malrotation.
In the older child or even adult presentation is more frequently intermittent with episodes of spontaneously resolving duodenal obstruction. This is thought to be due to kinking of the duodenum by Ladd bands rather than a volvulus 5. Internal hernias are also encountered.
In some individuals, the presentation is very non-specific, with recurrent episodes of abdominal pain and vomiting, diarrhea and weight loss, melena, or chronic pancreatitis 5.
Pathology
During normal embryogenesis, the bowel herniates into the base of the umbilical cord and rapidly elongates. As it returns to the abdominal cavity, it undergoes a complex ~270 degree counterclockwise rotation resulting in the duodenojejunal (DJ) flexure being typically located left of the midline, at the level of the L1 vertebral body, and the terminal ileum being located in the right iliac fossa. This results in a broad mesentery running obliquely down from the DJ flexure to the cecum and prevents rotation around the superior mesenteric artery (SMA) 1-6.
In malrotation, this does not occur and, as a result, the mesentery often has a short root, which can act as a pedicle (through which the SMA and superior mesenteric vein (SMV) pass) around which volvulus can occur.
The rotation of the duodenojejunal loop has been described as beginning around the 5th gestational week and completing around the 8th. Rotation of the cecocolic loop occurs at a later time, around the 10th week of gestational age. This could explain forms of partial intestinal malrotation 9.
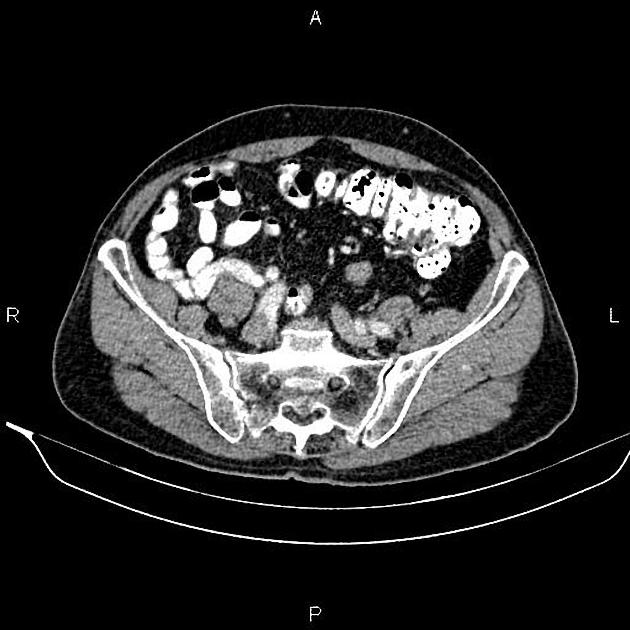
Intestinal non-rotation is a subtype of malrotation in which the small bowel is mainly located in the right hemiabdomen and the cecum in the left hemiabdomen. The risk of volvulus is much lower in complete non-rotation because patients have the effective anatomy of those who have undergone a Ladd procedure.
Radiographic features
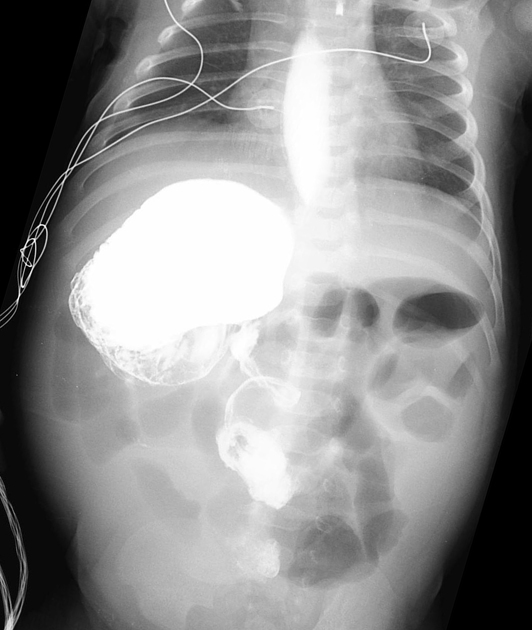
Plain radiograph
In the absence of midgut volvulus, abdominal radiographs are neither specific nor sensitive 2. They may show:
right-sided jejunal markings
absence of stool-filled colon in the right lower quadrant
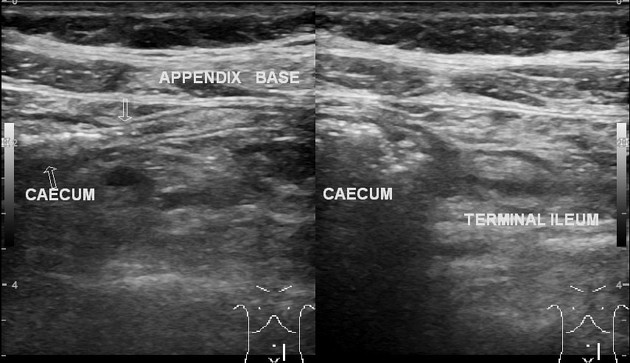
Ultrasound
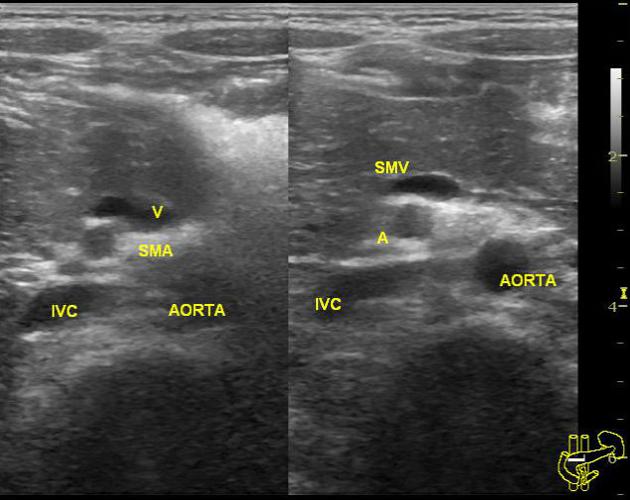
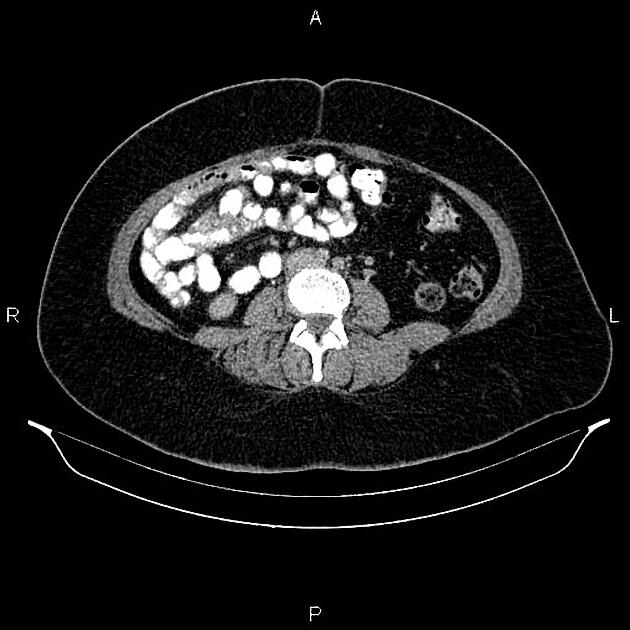
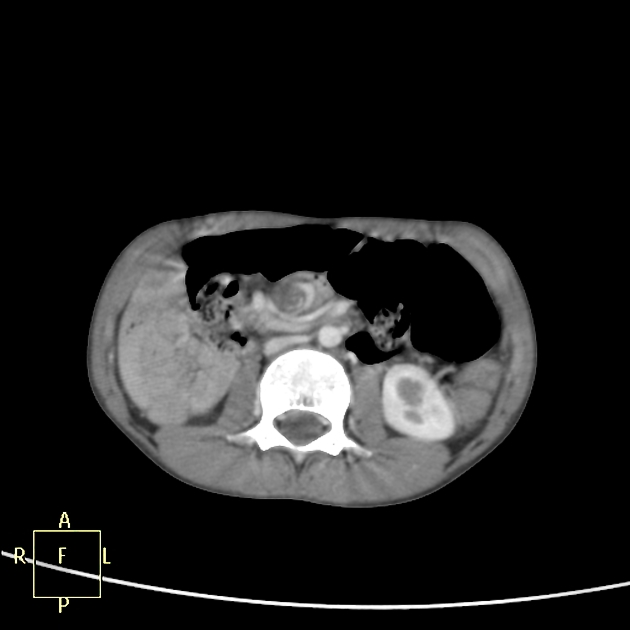
Inversion of the SMA/SMV relationship so the SMA lies on the right and the SMV on the left. Note however that this inverted relationship is seen in up to 11% of patients without malrotation, and a normal SMA/SMV relationship (SMA on left, SMV on right) can be seen in up to 29% of patients with surgically proven malrotation 9.
A more useful sign to rule out intestinal malrotation is the demonstration the retro-mesenteric D3 segment of the duodenum, where the horizontal (D3) segment of the duodenum should be seen in a transverse plane between the superior mesenteric vessels and the aorta 8,10,12.
Although demonstrating a retro-mesenteric duodenum is extremely sensitive and specific for excluding malrotation, it is not perfect and such a normal anatomic relationship has been described in at least one case of surgically treated intestinal malrotation with midgut volvulus 9. This case was likely secondary to partial intestinal malrotation, based on the embryological delay described above between the rotation of the duodenojejunal loop and the cecocolic loop.
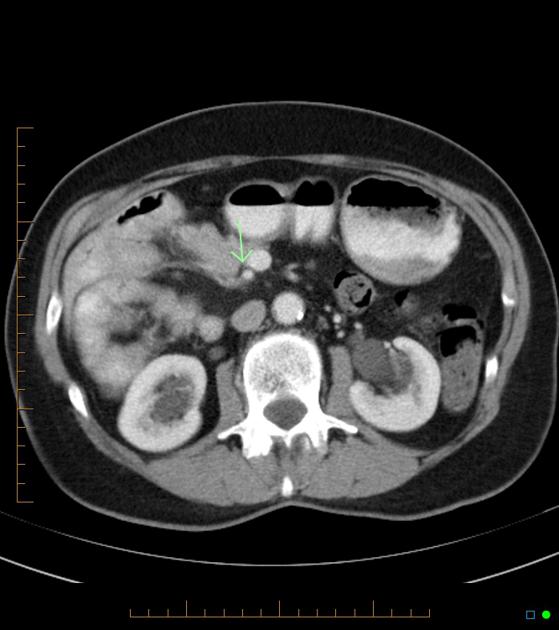
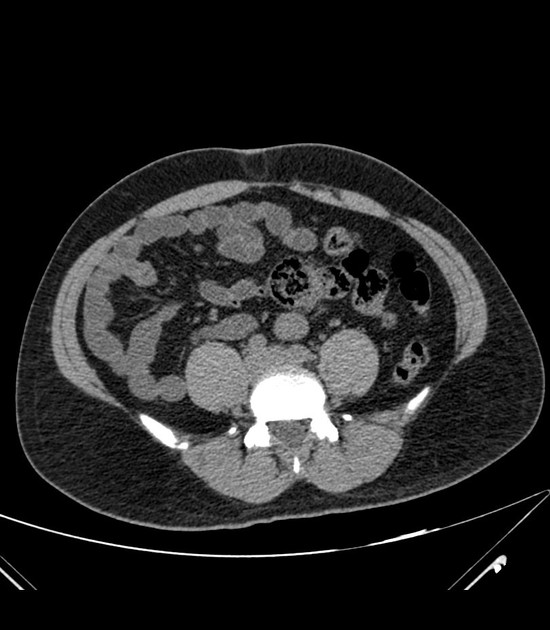
CT
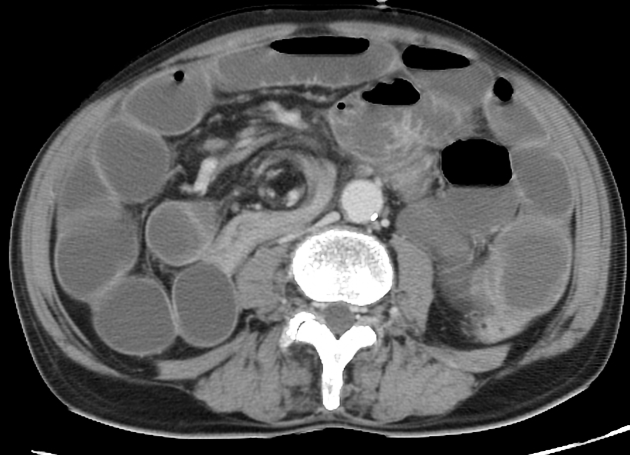
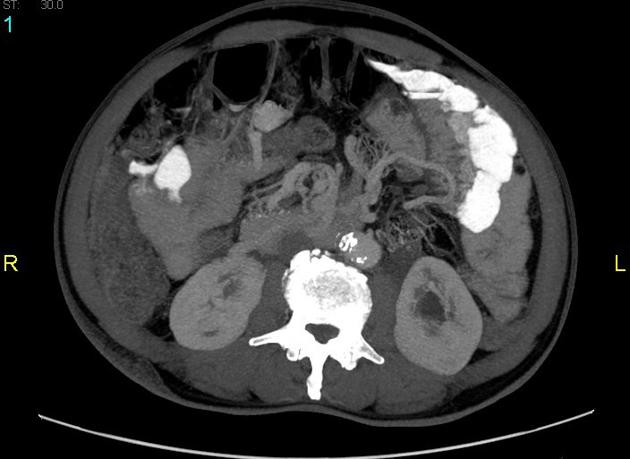
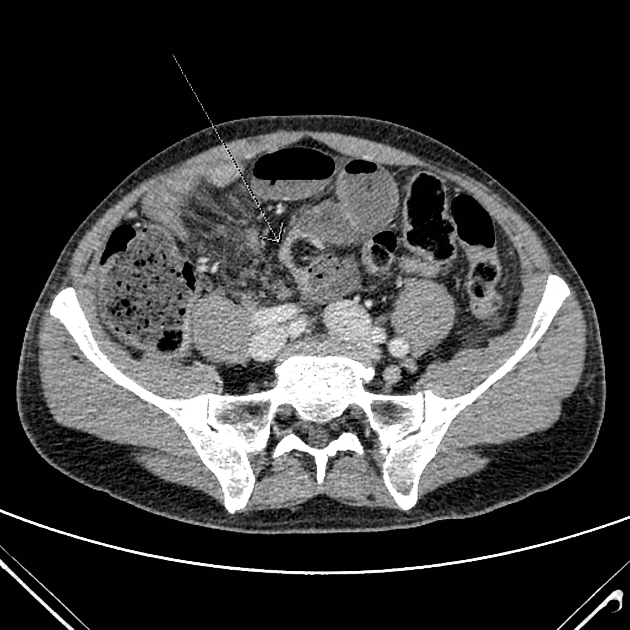
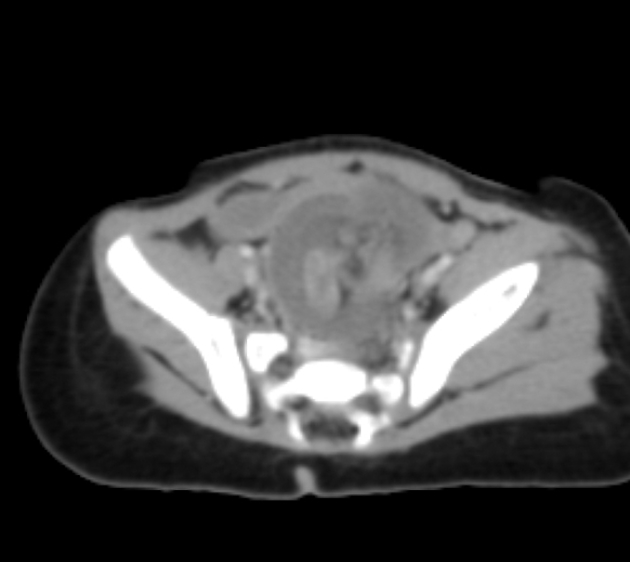
Depending on the degree of malrotation, CT may show:
absence of a retromesenteric (retroperitoneal) D3 segment of the duodenum 8
duodenojejunal junction inferior to the duodenal bulb in the right abdomen
abnormal SMA/SMV relationship (less reliable due to normal variation) 2
large bowel predominantly on the left and small bowel predominantly on the right
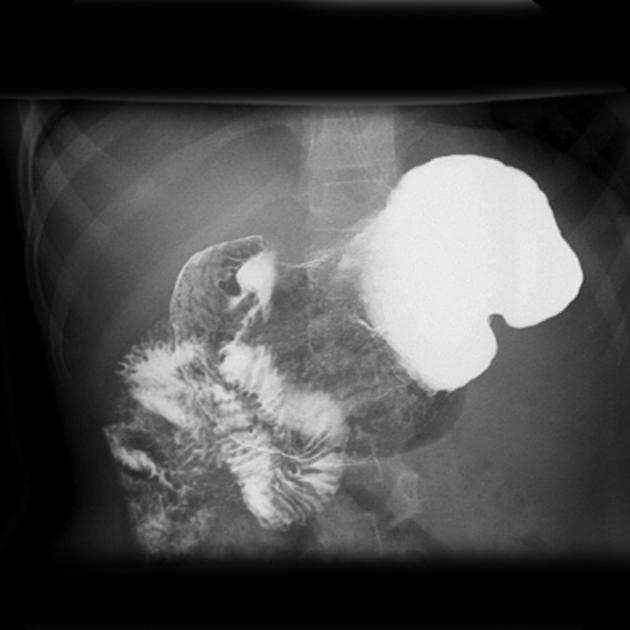
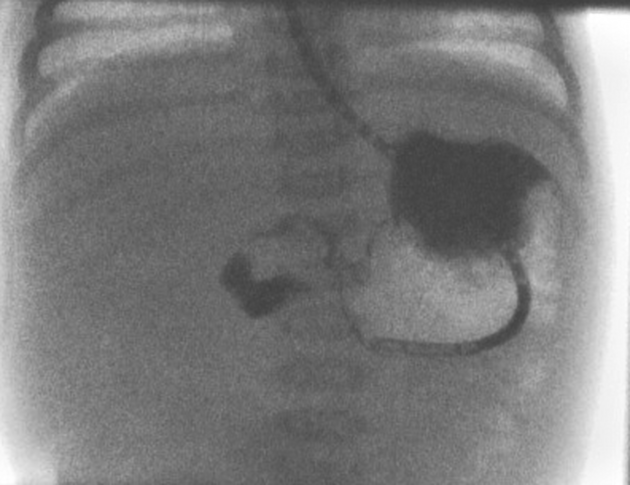
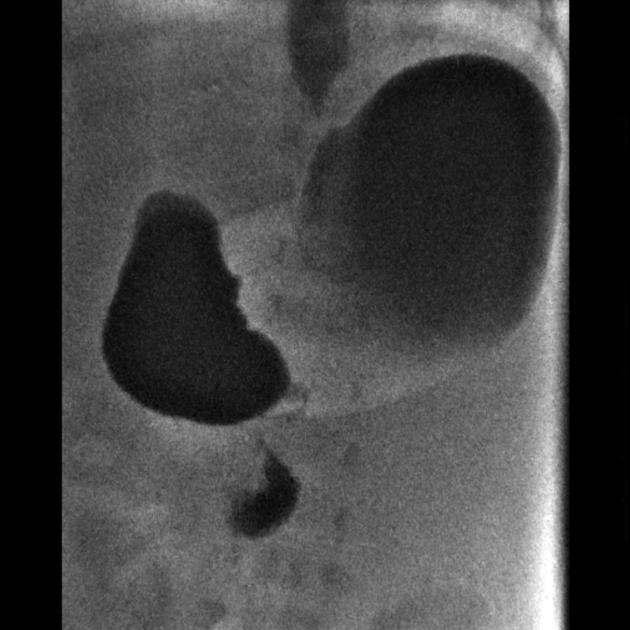
Fluoroscopy
A pediatric upper gastrointestinal contrast study is the examination of choice when the diagnosis is suspected. The key findings of malrotation is an abnormal duodenojejunal (DJ) junction location:
-
frontal view
DJ junction fails to cross the midline to the left of the left-sided vertebral body pedicle
DJ junction lies inferior to the duodenal bulb
-
lateral view
D2 and D3 segments of the duodenum not located posteriorly in a retroperitoneal position
Although not a specific criterion of malrotation, the jejunum will be commonly located to the right of the spine.
Contrast enema has historically also been used, the theory being that in malrotation the large bowel will also be malrotated. Unfortunately, in ~25% (range 20-30%) of cases with malrotation, the cecum is normally located. The converse is also true, with the position of the cecum in normal individuals being variable 4. Very rarely, the cecum may be malrotated and the small bowel in a normal position.
Treatment and prognosis
Due to the potential for life-threatening midgut volvulus and ischemic bowel, once discovered malrotation is often corrected surgically. The general principles of treatment are:
mobilization of the bowel including untwisting any volvulus present
division of abnormal peritoneal bands (Ladd bands)
widening of the mesenteric base
fixation of the duodenum and cecum to the retroperitoneum (pexy) is not universally performed 5,6
prophylactic appendectomy may be performed to avoid a subsequent missed diagnosis of appendicitis may occur (left sided abdominal pain)
Post-operatively the duodenum and small bowel remain on the right, and the cecum and colon are on the left side of the abdomen 5,6.
Differential diagnosis
A rate of 15% false positive has been reported in the diagnosis of malrotation using barium meal 7. Hence, differential diagnoses must be kept in mind, including:
normal duodenum: located inferiorly because of gastric distension or abnormally because of a feeding tube, renal agenesis, splenomegaly, etc.











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.