Duodenal atresia results from a congenital malformation of the duodenum and requires prompt correction in the neonatal period. It is considered to be one of the commonest causes of fetal bowel obstruction.
On this page:
Epidemiology
The prevalence of duodenal atresia is ~1 in 5,000-10,000 newborns, and there is no sex-associated difference in prevalence.
Associations
Associated conditions are common and include:
Down syndrome: ~30% of duodenal atresia cases may have Down syndrome while ~3% of Down syndrome cases may have duodenal atresia
VACTERL association
-
other intestinal atresias
Clinical presentation
Patients present in early life with duodenal obstruction and associated symptoms of abdominal distension, vomiting and absent bowel movements. In complete atresia, duodenum ends blindly with no communication with the distal bowel (and therefore no aeration distally). The atretic segment is usually just distal to the ampulla of Vater 1 and the child has bilious vomiting. If the atresia is proximal to the ampulla, the vomiting is non-bilious.
The vomiting usually occurs within the first 24 to 38 hours of neonatal life, typically following the first oral feeding and progressively worsens if not treated.
Pathology
Although more distal small bowel atresia is believed to be secondary to an ischemic episode, duodenal atresia is thought to represent a failure of recanalization of the bowel lumen that is a solid tube early in fetal life (~11-12 weeks).
In duodenal atresia, there is complete obstruction of the duodenal lumen, while in duodenal stenosis there is an incomplete obstruction of the duodenum lumen.
Radiographic features
Plain radiograph
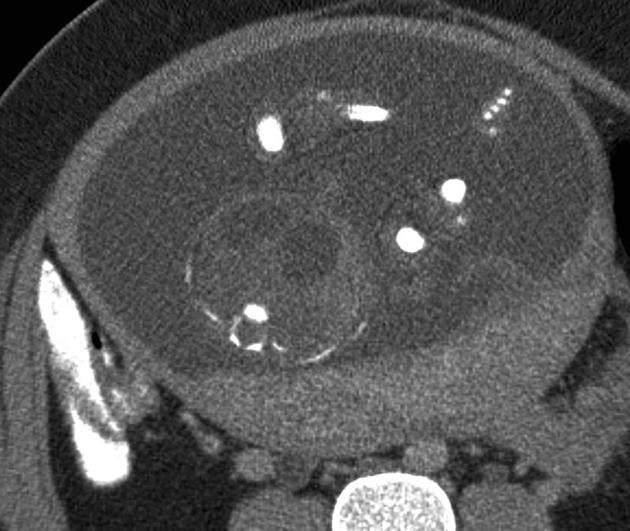
Abdominal radiographs may classically show a double bubble sign with gas filled distended stomach and duodenum with an absence of distal gas. A similar appearance (either filled with fluid or gas) can be seen in other modalities.
A double-bubble sign on an abdominal x-ray is a reliable indicator of duodenal atresia with even higher positive predictive value in patients with Down syndrome.
The presence of distal bowel gas, although more classically associated with duodenal stenosis, can be seen in duodenal atresia via anomalous bile duct anatomy 4.
Barium study
Barium contrast can be administered sometimes via an orogastric or nasogastric tube under fluoroscopy to evaluate the upper gastrointestinal tract. Only a controlled amount of barium is placed to confirm obstruction. It is then removed by nasogastric tube to prevent reflux and potential aspiration.
Ultrasound
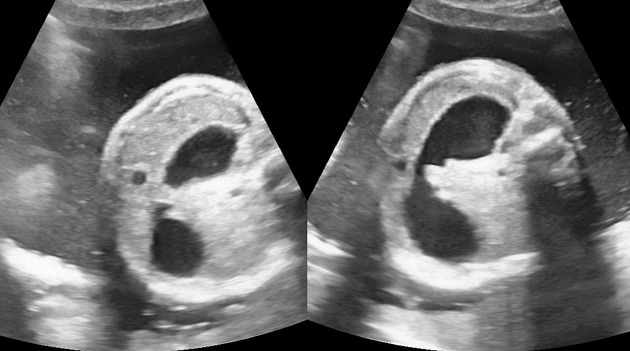
May also show a dilated stomach and duodenum giving a double bubble type appearance. This, however, may not be sonographically detectable until the mid to late second trimester. May also show evidence of polyhydramnios as an ancillary sonographic feature.
If a double-bubble sign is seen on antenatal ultrasound, then it is important to demonstrate a connection between the two fluid-filled structures because foregut duplication cyst, as well as other abdominal cysts, may simulate the appearance of a double-bubble sign.
Recognition that these structures are not continuous with the stomach will aid in the correct interpretation. This may occur in cases of choledochal cysts or renal, hepatic, omental, duplication or ovarian cysts. Likewise, a "double bubble" may be seen in cases of Ladd's bands, annular pancreas or volvulus, in which there is no duodenal atresia.
Treatment and prognosis
Surgical treatment for duodenal obstruction includes a number of different techniques for the intrinsic causes, including duodeno-duodenostomy and duodeno-jejunostomy. With surgical correction, prognosis is excellent (especially with isolated cases), and the outlook is therefore largely determined by other associated abnormalities.
Differential diagnosis
For plain radiograph appearances consider:
All three of these will show distal gas.
For an ultrasound appearance of a "double bubble" type appearance also consider:














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.