Midgut volvulus is a complication of bowel malrotation usually seen in neonates and infants. Presentation is usually with proximal small bowel obstruction and bilious vomiting. Without prompt treatment, there is a real and significant risk of small bowel ischemia, significant associated morbidity and even death.
On this page:
Epidemiology
Midgut volvulus can potentially occur at any age, but about 75% of cases occur within a month of birth 4,6. Most of these are within the first week 3, with 90% occurring in the under ones 6.
Clinical presentation
Typically, the neonate is entirely normal for a period and then suddenly presents with bilious vomiting.
Unless the volvulus is reduced (or reduces spontaneously), the superior mesenteric vein wrapped around the superior mesenteric artery causes progressive venous obstruction, gradual onset of ischemia, and eventual necrosis.
As this occurs, the abdomen becomes swollen and tender as fluid accumulates in the lumen of the bowel. Eventually, in severe, untreated cases, peritonitis and shock can result in severe morbidity and, sometimes, mortality.
Pathology
Midgut volvulus occurs as a complication of intestinal malrotation. Normal intestinal rotation results in:
a duodenal loop that crosses the midline
the DJ flexure to the left of midline at the level of the pylorus
central small bowel
the cecum in the right iliac fossa
peripheral large bowel
Malrotation describes the situation where this normal rotation is incomplete. NB intestinal non-rotation describes the complete absence of rotation and is not associated with an increased risk of volvulus.
The two important bits of anatomy here are the position of the DJ flexure and the position of the cecum because the small bowel mesenteric base sits between the two. In cases of malrotation, the DJ flexure is low and the cecum is usually high resulting in a short mesenteric root. The short root is a risk factor for volvulus in neonates and in cases of midgut volvulus, a short root is nearly always seen.
Radiographic features
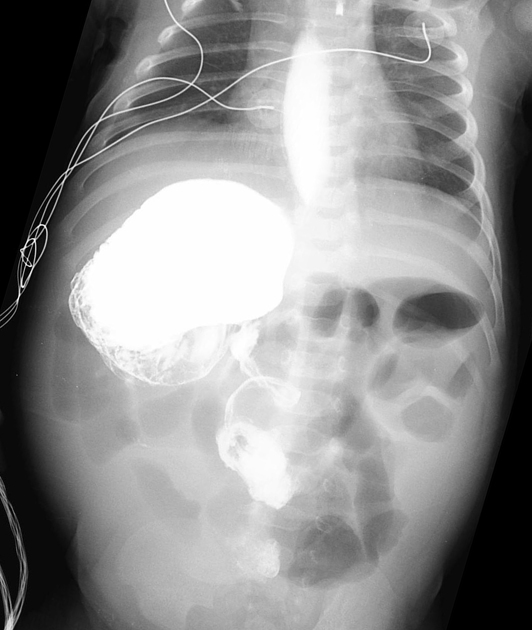
Plain radiograph
Plain radiograph findings are nonspecific. They may be normal early on, or show developing bowel obstruction as time progresses. Later, in untreated patients, they may show pneumoperitoneum where obstructed, ischemic bowel perforates.
Occasionally complete obstruction can lead to distension of the duodenal bulb and stomach leading to a double bubble sign 7.
Fluoroscopy
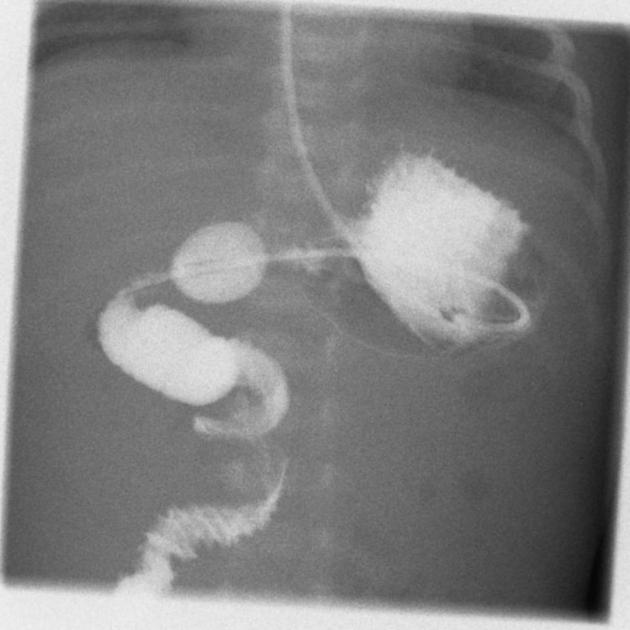
A pediatric upper gastrointestinal contrast study is the examination of choice when the diagnosis is suspected. Not only is it able to identify the volvulus, but even in instances where spontaneous reduction has occurred, the underlying malrotation will be evident.
In the setting of volvulus findings include:
tapering or beaking of the bowel in complete obstruction 3
malrotated bowel configuration
Contrast enemas have also been used historically. The theory being that in malrotation the large bowel will also be malrotated. Unfortunately, in 20-30% of cases, the cecum is normally located. The converse is also true, with the position of the cecum in normal individuals being variable 3.
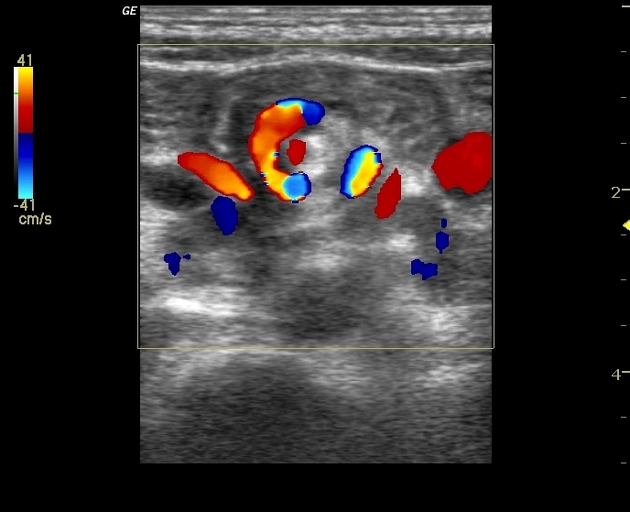
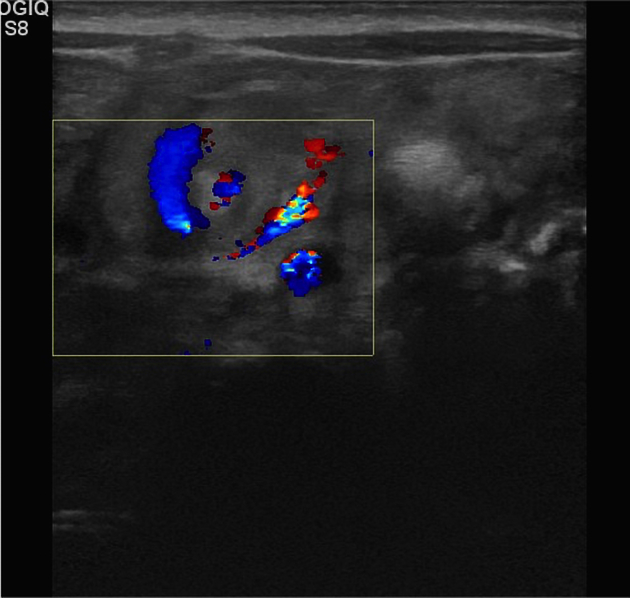
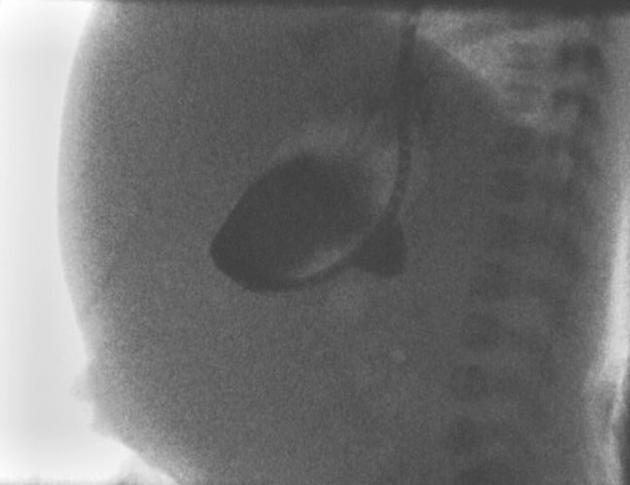
Ultrasound
Ultrasound is helpful when volvulus is confidently identified. Findings in volvulus include 1-5:
clockwise whirlpool sign
-
abnormal superior mesenteric vessels
inverted SMA/SMV relationship
solitary hyperdynamic pulsating SMA
truncated SMA
inapparent SMV
-
abnormal bowel
dilated duodenum proximal to the obstruction
thickened wall of small bowel distal to the obstruction
dilated fluid-filled loops of small bowel
free intra-abdominal fluid
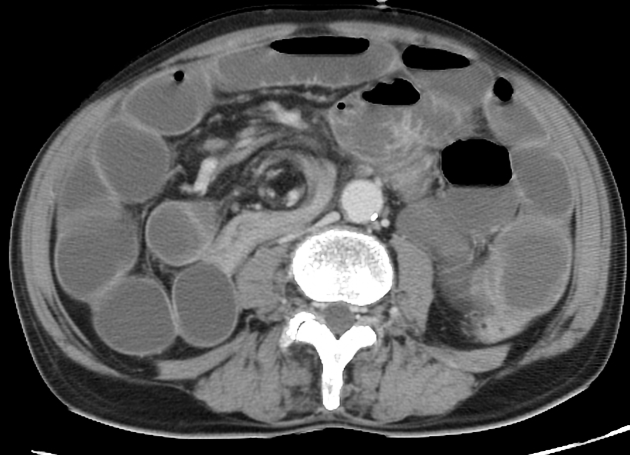
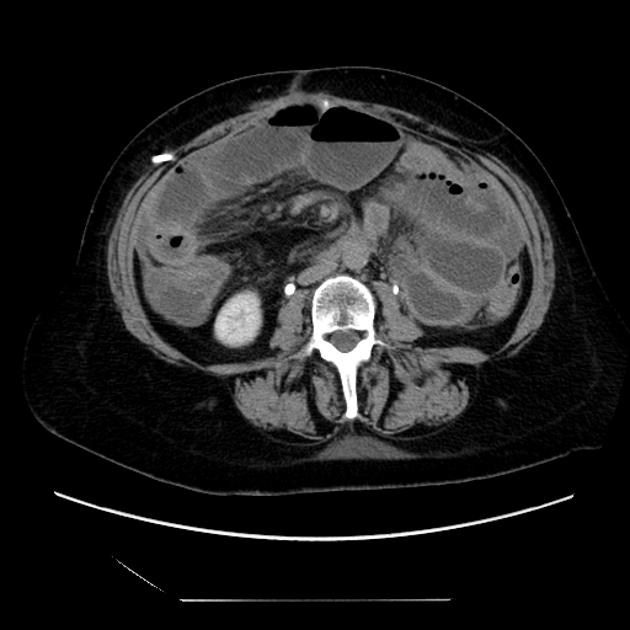
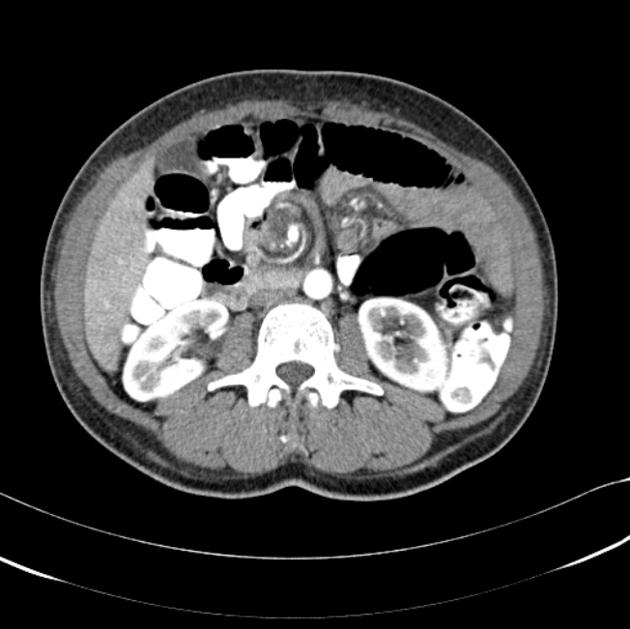
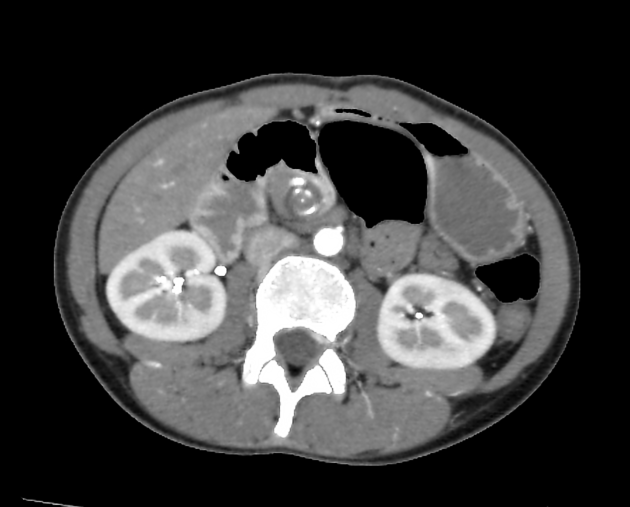
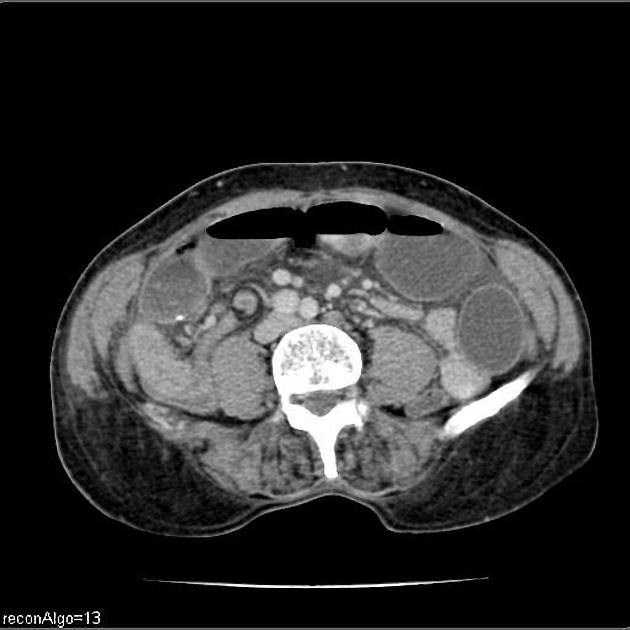
CT
CT is often carried out in older patients, in which presentation is non-specific.
Findings include:
whirlpool sign of twisted mesentery
malrotated bowel configuration
inverted SMA/SMV relationship
bowel obstruction
free fluid/free gas in advanced cases
Treatment and prognosis
Urgent resuscitation and surgical intervention is required in confirmed or suspected midgut volvulus.
Surgically, the bowel is devolved to allow restoration of blood supply and resection of any non-viable loops is performed (Ladd procedure). If resection is performed stomas are usually created. Ladd bands are divided and the mesenteric pedicle widened. In some instances, pexy (surgical fixation) of the duodenum and cecum may be performed although it is unclear if this is of benefit in preventing recurrence 6.
It should be noted that normal anatomical positioning is not achieved; the duodenum and small bowel remain on the right, and the cecum and colon are on the left side of the abdomen 6.
Prognosis is dependent on the state of the small bowel and presence of systemic shock. In cases where no ischemia of the bowel is present, and the child is otherwise well, the prognosis is extremely good. Overall mortality of 3-9% is reported 6.
Small bowel obstruction for adhesions is seen as a distant complication in 5-10% of cases.
Differential diagnosis
Vomiting in infancy has numerous causes and needs to be distinguished from normal possetting. Differential of a proximal obstruction includes 3,6,7:
pyloric stenosis: vomiting will be non-bilious and projectile
-
congenital obstruction
-
external compression of the duodenum
intramural duodenal hematoma
retroperitoneal tumor










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.