Intracranial epidural abscess, less commonly called epidural empyema, refers to a pyogenic collection within the epidural space of the head. Spinal epidural abscess is discussed separately.
Similarly to subdural empyemas, sinusitis is the most common cause of intracranial epidural abscesses.
On imaging, it tends to present as an epidural collection of biconvex shape, usually not crossing the suture lines, and with marked meningeal enhancement. On MRI, typically demonstrates restricted diffusion.
On this page:
Epidemiology
Epidural abscesses are rare overall but together with subdural empyema account for around 20-33% of all intracranial infections. They can present in any age group and have no real gender predilection.
Clinical presentation
Epidural abscess presents similar to other intracranial infections with:
- fever
- headache
- nuchal rigidity
- focal neurologic deficits or seizures may also occur in cases of large space-occupying empyemas
Patients may also have active sinusitis, with epidural abscess being a potential complication of the condition.
Pathology
The most commonly isolated pathogens are Streptococci pneumoniae, Haemophilus influenzae, Staphylococcus aureus and Staphylococcus epidermidis.
In more than two-thirds of cases, an epidural abscess is a complication of sinusitis. Seeding can be via direct invasion through the sinus walls or hematogenous seeding through retrograde valveless bridging veins.
Another significant cause is mastoiditis which accounts as the cause in approximately 20% of cases. Epidural abscesses can also occur as a result of trauma, epidural injections or anesthesia, open head or spinal trauma, neurosurgery or meningitis.
Radiographic features
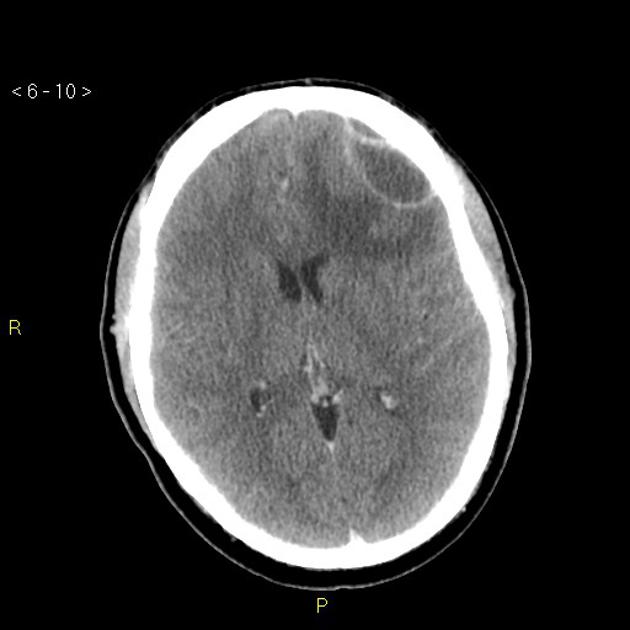
CT
CT is less sensitive for the detection of epidural abscess compared to MRI. Features on CT include:
- extra-axial location
- isodense or hypodense to surrounding brain
- biconvex shape
- usually do not cross suture lines
- may cross the midline
- strong peripheral enhancement with contrast
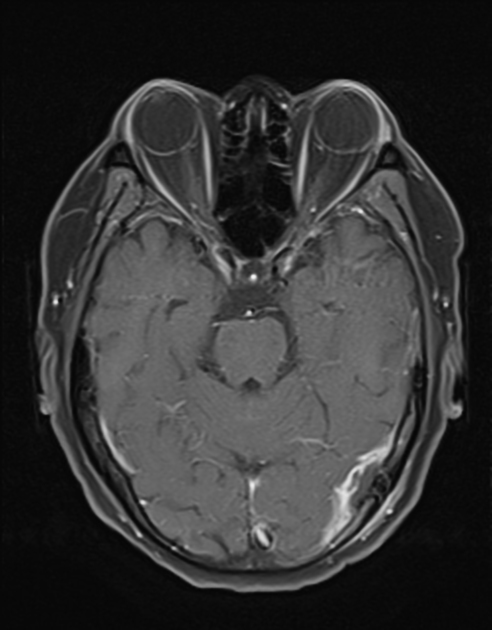
MRI
Characteristics on MRI include:
- T1: hyperintense
- T1 C+ (Gd): strong peripheral contrast enhancement
- T2/FLAIR: isointense or hyperintense
- PD: isointense or hyperintense
- DWI: area of restricted diffusion
Treatment and prognosis
Prompt recognition and surgical evacuation of the collection is essential to the management of epidural abscess. It may be fatal in up to 15% of cases.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.