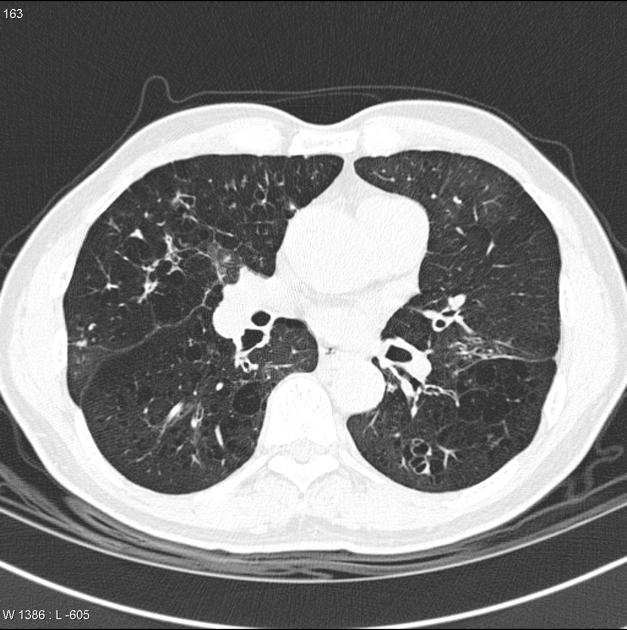
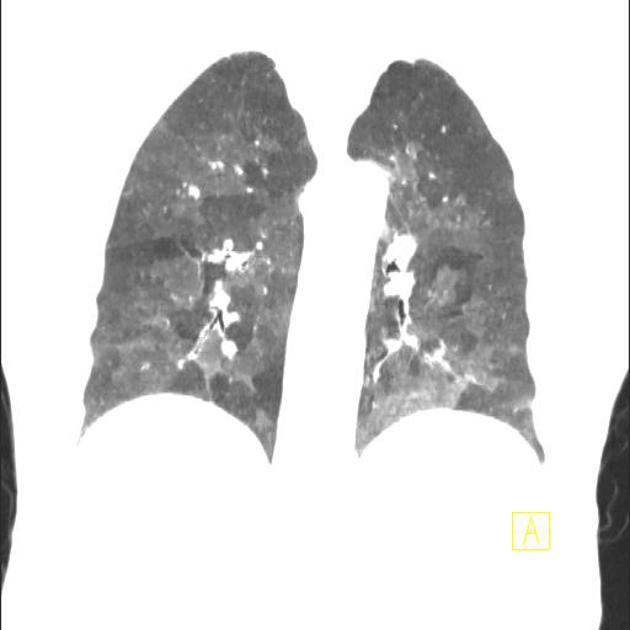
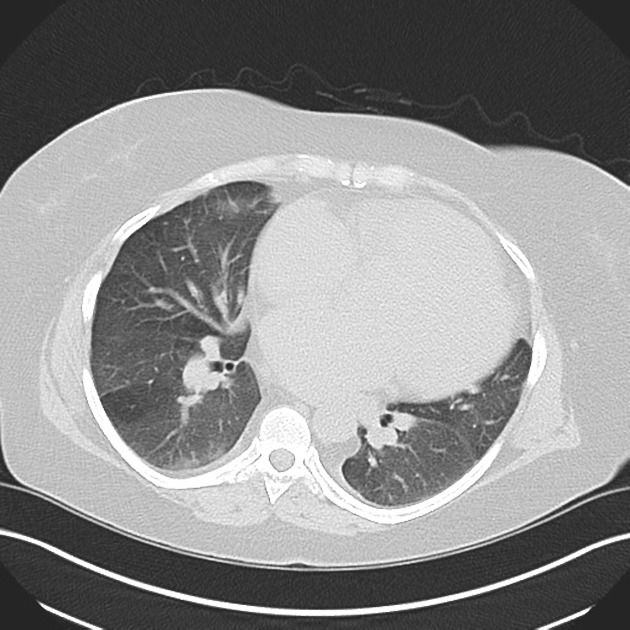
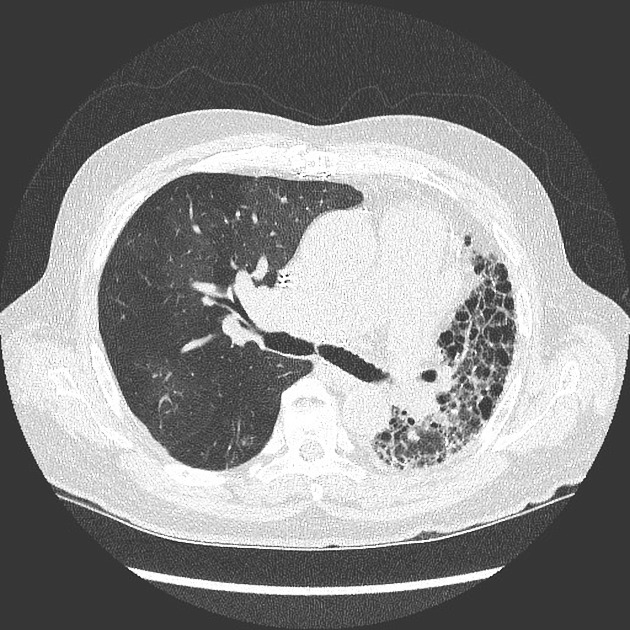
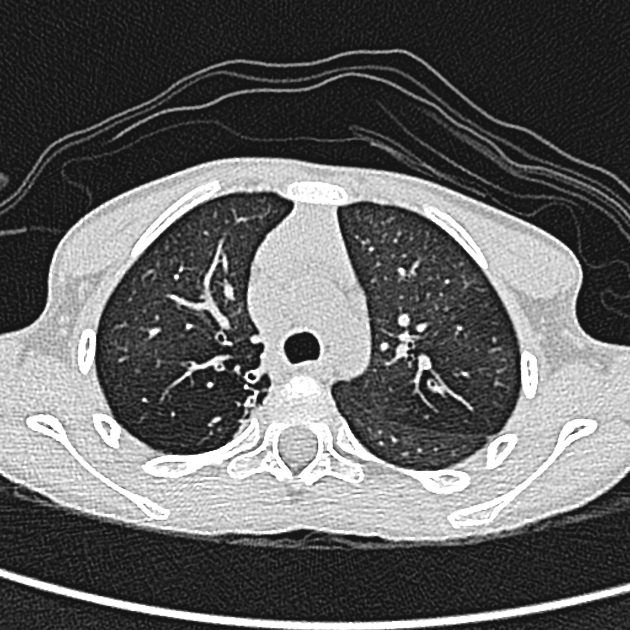
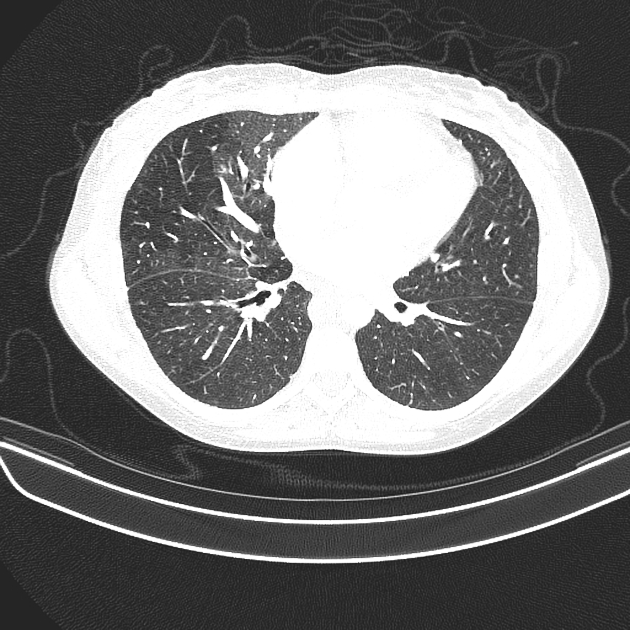
Mosaic attenuation pattern in lung
Citation, DOI, disclosures and article data
At the time the article was created Nick Henson had no recorded disclosures.
View Nick Henson's current disclosuresAt the time the article was last revised Liz Silverstone had no financial relationships to ineligible companies to disclose.
View Liz Silverstone's current disclosures- Mosaic oligemia
- Mosaic oligaemia
- Mosaic attenuation pattern
- Mosaic attenuation
- Mosaic perfusion pattern
- Mosaic attenuation pattern in lungs
- Mosaic attenuation pattern in the lung
- Mosaic perfusion
Mosaic attenuation describes a CT pattern that comprises a patchwork of regions of differing pulmonary attenuation. The term can only be applied to CT acquired during full inspiration 17. Causes fall into the following categories:
obliterative small airways disease: regional air-trapping causes abnormally low attenuation, exacerbated by reflex vasoconstriction. Low attenuation is maintained on expiratory CT in contrast to the increased attenuation of normal lung. Relative hyperaemia can increase attenuation in unaffected areas 5,10. Causes include bronchiectasis, constrictive bronchiolitis and hypersensitivity pneumonitis
occlusive vascular disease causes mosaic perfusion 7: low attenuation regions are oligaemic and normal areas may be hyperaemic, with increased attenuation. Attenuation of all regions increases on expiration. Chronic thromboembolic pulmonary hypertension is a common cause.
-
multifocal disease causing ground glass opacity in a mosaic pattern is commonly (about 50% 5) due to
acute pulmonary oedema 10
-
a combination of normal lung, air trapping and ground glass opacity:
hypersensitivity pneumonitis, a three density pattern is characteristic
Differentiating the cause
Although "mosaic attenuation" is non-specific, a radiologist should search for ancillary imaging findings which may help identify the underlying process in order to help guide clinical management.
Ascertaining the underlying cause for mosaic attenuation is often possible on the basis of clinical information, combined with the assessment of other lung features on HRCT 2,5:
peripheral vessels: if vessels in hypoattenuated regions of the lung are smaller than in the other regions, the pattern is due to mosaic perfusion (i.e. airways or vascular disease rather than ground-glass)
central vessels: pulmonary hypertension, reflected as dilatation of the central pulmonary arteries, suggests a vascular cause
small airways: the presence of abnormally dilated or thick walled airways in the relatively lucent lung confirms underlying airway disease, see small airways disease
parenchymal changes: ground glass opacity is the likely cause for mosaic attenuation if other features of the infiltrative disease are present, such as reticular opacities (i.e. crazy paving pattern) or nodules
air trapping: refers to regions of the lung which following expiration do not show the normal increase in attenuation, or show little change in cross-sectional area 5 (i.e. this is an expiratory HRCT finding); the presence of air trapping suggests airway disease
A practical approach to the aetiological diagnosis of a mosaic attenuation pattern is to ask the following question: 'Which is the pathological lung area?' 5,10
-
Is the abnormal lung hyperattenuating?
parenchymal lung disease (most common cause, 50%)
pulmonary oedema
pulmonary haemorrhage
-
Is the abnormal lung area hypoattenuating?
occlusive vascular disease (oligaemia)
obstructive small airways disease (air-trapping plus secondary vasoconstriction)
Quiz questions
References
- 1. Hansell DM, Bankier AA, Macmahon H et-al. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008;246 (3): 697-722. doi:10.1148/radiol.2462070712 - Pubmed citation
- 2. Arakawa H, Niimi H, Kurihara Y et-al. Expiratory high-resolution CT: diagnostic value in diffuse lung diseases. AJR Am J Roentgenol. 2000;175 (6): 1537-43. AJR Am J Roentgenol (full text) - Pubmed citation
- 3. Sherrick AD, Swensen SJ, Hartman TE. Mosaic pattern of lung attenuation on CT scans: frequency among patients with pulmonary artery hypertension of different causes. AJR Am J Roentgenol. 1997;169 (1): 79-82. AJR Am J Roentgenol (abstract) - Pubmed citation
- 4. Stern EJ, Swensen SJ, Hartman TE et-al. CT mosaic pattern of lung attenuation: distinguishing different causes. AJR Am J Roentgenol. 1995;165 (4): 813-6. AJR Am J Roentgenol (abstract) - Pubmed citation
- 5. Webb WR, Műller NL, Naidich DP. High-resolution CT of the lung. Lippincott Williams & Wilkins. (2008) ISBN:0781769094. Read it at Google Books - Find it at Amazon
- 6. Ridge CA, Bankier AA, Eisenberg RL. Mosaic attenuation. AJR Am J Roentgenol. 2011;197 (6): W970-7. doi:10.2214/AJR.11.7067 - Pubmed citation
- 7. Elicker BM, Webb WR. Fundamentals of High-Resolution Lung Ct. Lippincott Williams & Wilkins. (2013) ISBN:1451184085. Read it at Google Books - Find it at Amazon
- 8. Stern EJ, Müller NL, Swensen SJ et-al. CT mosaic pattern of lung attenuation: etiologies and terminology. J Thorac Imaging. 1996;10 (4): 294-7. Pubmed citation8.
- 9. Suga K, Yasuhiko K, Iwanaga H et-al. Functional mechanism of lung mosaic CT attenuation: assessment with deep-inspiration breath-hold perfusion SPECT-CT fusion imaging and non-breath-hold Technegas SPECT. Acta Radiol. 2009;50 (1): 34-41. doi:10.1080/02841850802575628 - Pubmed citation
- 10. Kligerman SJ, Henry T, Lin CT, Franks TJ, Galvin JR. Mosaic Attenuation: Etiology, Methods of Differentiation, and Pitfalls. Radiographics : a review publication of the Radiological Society of North America, Inc. 35 (5): 1360-80. doi:10.1148/rg.2015140308 - Pubmed
- 11. Kasai H, Tanabe N, Fujimoto K, Hoshi H, Naito J, Suzuki R, Matsumura A, Sugiura T, Sakao S, Tatsumi K. Mosaic attenuation pattern in non-contrast computed tomography for the assessment of pulmonary perfusion in chronic thromboembolic pulmonary hypertension. (2017) Respiratory investigation. 55 (5): 300-307. doi:10.1016/j.resinv.2017.07.003 - Pubmed
- 12. Chung JH, Zhan X, Cao M, Koelsch TL, Manjarres DCG, Brown KK, Lynch DA, Russell G, Fernández Pérez ER. Presence of Air Trapping and Mosaic Attenuation on Chest Computed Tomography Predicts Survival in Chronic Hypersensitivity Pneumonitis. (2017) Annals of the American Thoracic Society. 14 (10): 1533-1538. doi:10.1513/AnnalsATS.201701-035OC - Pubmed
- 13. Ussavarungsi K, Lee AS, Burger CD. Mosaic Pattern of Lung Attenuation on Chest CT in Patients with Pulmonary Hypertension. (2015) Diseases (Basel, Switzerland). 3 (3): 205-212. doi:10.3390/diseases3030205 - Pubmed
- 14. Barnett J, Molyneaux P, Rawal B et al. Variable Utility of Mosaic Attenuation To distinguish Fibrotic Hypersensitivity Pneumonitis from Idiopathic Pulmonary Fibrosis. Eur Respir J. 2019;54(1):1900531. doi:10.1183/13993003.00531-2019 - Pubmed
- 15. Khalid F, Rehman S, Gupta S. Eighty-Five-Year-Old Man with Mosaic Attenuation on Chest Imaging. BMJ Case Rep. 2018;2018:bcr-2017-222644. doi:10.1136/bcr-2017-222644 - Pubmed
- 16. Lee G, Carroll M, Galvin J, Walker C. Mosaic Attenuation Pattern: A Guide to Analysis with HRCT. Radiol Clin North Am. 2022;60(6):963-78. doi:10.1016/j.rcl.2022.06.009 - Pubmed
- 17. Bankier A, MacMahon H, Colby T et al. Fleischner Society: Glossary of Terms for Thoracic Imaging. Radiology. 2024;310(2):e232558. doi:10.1148/radiol.232558 - Pubmed
Incoming Links
- Chest curriculum
- Pulmonary veno-occlusive disease
- Small airways disease
- Sickle cell disease (acute chest syndrome)
- Crohn disease
- Mosaic attenuation pattern in lung
- Tropical pulmonary eosinophilia
- Diffuse panbronchiolitis
- Three attenuation pattern
- Chronic thromboembolic pulmonary hypertension
- Non-fibrotic hypersensitivity pneumonitis
- Cystic fibrosis (pulmonary manifestations)
- Non-specific interstitial pneumonia
- Mosaic appearance (disambiguation)
- Pulmonary Langerhans cell histiocytosis
- Pulmonary hypertension
- Inanimate object inspired signs
- Acute hypersensitivity pneumonitis (historical)
- Bronchiolitis
- Post-lung transplant bronchiolitis obliterans
- Chronic pulmonary embolism
- Patent ductus arteriosus
- Exogenous lipoid pneumonia
- Allergic bronchopulmonary aspergillosis (ABPA)
- Obliterative bronchiolitis in a lung transplant
- Ground-glass opacification due to COVID-19 infection
- Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH)
- Roman mosaic
- Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia with pulmonary carcinoid tumour
- Bronchiolitis obliterans
- Mosaic attenuation of lung parenchyma
- Saddle pulmonary embolism
- Swyer-James syndrome
- Cystic bronchiectasis
- Mosaic attenuation pattern (pulmonary hypertension)
- Fibrotic hypersensitivity pneumonitis
- Cystic fibrosis
- Cystic bronchiectasis
- Cystic fibrosis
- Pneumocystis carinii pneumonia
Related articles: Inspired signs
-
inanimate object inspired
- accordion sign
- astronomical inspired
- ball of wool sign
- ball on tee sign (renal papillary necrosis)
- boot-shaped heart
- bowler hat sign
- bow tie sign
- box-shaped heart
- bucket handle appearance (disambiguation)
- chain of lakes sign
- champagne glass pelvis
- cobblestone appearance
- Coca-Cola bottle sign
- cockade sign (disambiguation)
- coin lesion
- collar button ulcer
- comb sign
- corduroy artifact
- corduroy sign
-
corkscrew sign (disambiguation)
- corkscrew sign (diffuse oesophageal spasm)
- corkscrew sign (inner ear)
- corkscrew sign (midgut volvulus)
- crazy paving sign
- cupola sign
- curtain sign (lung ultrasound)
- dinner fork deformity
- dripping candle wax sign
- finger in glove sign
- fishhook ureters
- flame-shaped breast (gynaecomastia)
- football sign (pneumoperitoneum)
- frozen pelvis
- ghost triad (gallbladder)
- ghost vertebra
- goblet sign
- ground glass opacity
- hockey stick sign (disambiguation)
- horseshoe (disambiguation)
- hourglass sign
- hurricane sign (cardiac SPECT)
- jail bar sign
- keyhole sign (disambiguation)
- leather bottle stomach
- light bulb sign (disambiguation)
- Lincoln log vertebra
- Mercedes-Benz sign (disambiguation)
- misty mesentery sign
- mosaic appearance (disambiguation)
- napkin ring sign
- open book fracture
- pearl necklace sign
- pencil in a cup
- picture frame vertebral body
- polka-dot sign
- rachitic rosary
- ribbon rib deformity
- ring shadow
- rugger jersey spine
- sack of marbles sign
- sail sign (disambiguation)
- scalpel sign
- spilt teacup sign
- stepladder sign (disambiguation)
-
string of pearls sign (disambiguation)
- string of pearls sign (abdominal radiograph of small bowel)
- string of pearls sign (polycystic ovarian syndrome)
- string of pearls sign (fibromuscular dysplasia)
- string of pearls sign (watershed infarction)
- Tam o' Shanter sign
- telephone receiver deformity
- thimble bladder
- tombstone iliac wings
- Venetian blind sign
- Venus necklace sign
- water bottle sign
-
weapon and munition inspired signs
- arrowhead sign
- bayonet artifact
- bayonet deformity
- boomerang sign (disambiguation)
- bullet-shaped vertebra
- cannonball metastases
- Cupid bow contour
- dagger sign
- double barrel sign
- halberd pelvis
- hatchet sign
- panzerherz
- pistol grip deformity
- saber-sheath trachea
- scimitar syndrome
-
target sign (disambiguation)
- double target sign (hepatic abscess)
- eccentric target sign (cerebral toxoplasmosis)
- reverse target sign (cirrhotic nodules)
- target sign (cholangiocarcinoma)
- target sign (choledocholithiasis)
- target sign (hepatic metastases)
- target sign (intussusception)
- target sign (neurofibromas)
- target sign (pyloric stenosis)
- target sign (tuberculosis)
- trident appearance
- Viking helmet sign
- white pyramid sign
- windswept knees
- wine bottle sign
-
vegetable and plant inspired
- aubergine sign
- bamboo spine
- blade of grass sign
- celery stalk appearance (disambiguation)
- coconut left atrium
- coffee bean sign
- cotton wool appearance
- drooping lily sign
- ginkgo leaf sign (disambiguation)
- holly leaf sign
- iris sign
- ivy sign
- miliary opacities
- mistletoe sign
- onion signs (disambiguation)
- pine cone bladder
-
popcorn calcification (disambiguation)
- popcorn calcification (breast)
- popcorn calcification (chondroid lesions)
- popcorn calcification (fibrous dysplasia)
- popcorn calcification (osteogenesis imperfecta)
- popcorn calcification (pulmonary hamartomas)
- popcorn calcification (uterine fibroid)
- potato nodes
- rice signs (disambiguation)
- salt and pepper sign (disambiguation)
- tombstone iliac wings
- tree-in-bud
- tulip sign
- water lily sign
-
fruit inspired
- apple core sign (disambiguation)
- apple-peel intestinal atresia
- banana and egg sign
- banana fracture
- banana sign
- berry aneurysm
- bowl of grapes sign
-
bunch of grapes sign (disambiguation)
- bunch of grapes sign (hydatidiform mole)
- bunch of grapes sign (bronchiectasis)
- bunch of grapes sign (IPMN)
- bunch of grapes sign (botryoid rhabdomyosarcoma)
- bunch of grapes sign (intracranial tuberculoma)
- bunch of grapes sign (intraosseous haemangiomas)
- bunch of grapes sign (multicystic dysplastic kidney)
- cashew nut sign
- lemon sign
- pear-shaped bladder
- strawberry gallbladder
- strawberry skull
- watermelon skin sign
-
animal and animal produce inspired
- human
- mammals
- anteater nose sign
- antler sign
- batwing opacities
- bear paw sign
- beaver tail liver
- Brahma bull sign
- buffalo chest
- bull's eye sign (disambiguation)
- bunny waveform sign
- claw sign
- dog ear sign
- dog leg sign
- dromedary hump
- ears of the lynx sign
- eye of tiger sign
- feline oesophagus
- giraffe pattern
- hidebound sign
- ivory phalanx
- ivory vertebra sign
- joint mouse
- leaping dolphin sign
- leopard skin sign
- moose head appearance
- panda sign
- piglet sign
- pleural mouse
- raccoon eyes sign
- rat bite erosions
- rat-tail sign
- Scottie dog sign
- Snoopy sign
- stag's antler sign
- staghorn calculus
- tiger stripe sign
-
zebra sign (disambiguation)
- zebra sign: (cerebellar haemorrhage)
- zebra spleen: arterial phase (spleen)
- zebra stripe sign (osteogenesis imperfecta)
- amphibians
- birds
- bird beak sign (disambiguation)
- bird's nest sign (lung)
- crow feet sign
- egg on a string sign
- eggshell calcification (breast)
- eggshell calcification (lymph nodes)
- gooseneck sign (endocardial cushion defect)
- gull wing appearance
- hummingbird sign
- owl eyes sign
- pooping duck sign
- sitting duck appearance
- swallowtail sign
- swan neck deformity
- winking owl sign
- fish and marine life
- reptiles
- arthropods
- micro-organisms
- fictional creatures
-
food inspired
- Cheerio sign (disambiguation)
- chocolate cyst
- cottage loaf sign
- double Oreo cookie (glenoid labrum)
- doughnut sign (disambiguation)
- hamburger sign (spine)
- head cheese sign (lungs)
- honeycombing (lungs)
- hot cross bun sign (pons)
- ice cream cone sign (middle ear ossicles)
- ice cream cone sign (vestibular schwannoma)
- licked candy stick appearance (bones)
- linguine sign (breast implants)
- macaroni sign
- omental cake
- Oreo cookie (heart)
- pancake organ (disambiguation)
- Polo mint sign
- salad oil sign (breast implants)
- sandwich sign (disambiguation)
- sandwich vertebra
- sausage digit
- spaghetti sign
- Swiss cheese sign
-
alphabet inspired
- A line (US artifact)
- C sign (MSK)
- delta sign (disambiguation)
- E sign
- H-shaped vertebra
- H sign
- J-shaped sella
- J sign (shoulder)
- L sign (brain)
- lambda sign (disambiguation)
- M sign
- omega epiglottis
- O sign (gastric banding)
- P sign (epiglottis)
- S sign of Golden
- tau sign
- T sign (disambiguation)
- U fibres
- U-figure (pelvis)
- U sign (brain)
- V sign (disambiguation)
- W hernia
- X-marks-the-spot sign
- Y sign (epidural lipomatosis)
- Z deformity
-
Christmas inspired
- Christmas tree bladder in neurogenic bladder
- holly leaf sign in calcified pleural plaques
- ivy sign in leptomeningeal enhancement
- nutcracker oesophagus in oesophageal dysmotility
- shepherd's crook deformity of the femur in fibrous dysplasia
- snowcap sign in avascular necrosis
- snowman sign (disambiguation)
- snowstorm appearance in complete hydatidiform mole and testicular microlithiasis
- miscellaneous







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.