Non-ischemic cerebral enhancing (NICE) lesions are an uncommon delayed complication of cerebrovascular procedures, including aneurysm coiling, thrombectomy and placement flow-diverter stent placement 1,2,4,5.
On this page:
Epidemiology
As NICE lesions are seen following endovascular procedures most commonly for aneurysm treatment, the epidemiology of cases mirrors that of cerebral aneurysms. Reported cases vary in age from 31 to 71 years 1.
The incidence of NICE lesions in patients who have undergone aneurysm coiling is reported as approximately 0.5% 1,2 although, given the low number of reported cases and the potential for many cases being unrecognised, the true incidence is unknown.
There appears to be a female predilection 1.
Clinical presentation
NICE lesions are a delayed phenomenon and typically present many days to weeks following the procedure; reported range: 2 weeks to 12 months 1,2,4,5. Symptoms are variable depending on the location and number of lesions 1,5.
CSF examination is usually bland or demonstrates mild elevation of protein and white cells 1,2.
Pathology
The cause of NICE lesions remains somewhat controversial with most authors believing that they represent a granulomatous reaction to foreign body emboli occurring at the time of intervention 1,2. An alternative theory is that they are the result of nickel hypersensitivity, less favored as many endovascular catheters and devices are made of other alloys (e.g. cobalt-chromium) 1,5.
In some reported cases where biopsy was undertaken, histology demonstrated foreign-body granulomatous reaction surrounding sterile microabscess containing fragments of the hydrophilic coating of many catheters, such as polyvinylpyrrolidone (PVP) 2,5. Similar reactions have been identified in other parts of the body (e.g. the wrist from radial puncture in coronary angiograms) 1.
It has been postulated that the risk of developing NICE lesions is related to tight-fitting catheter/guidewire/device combinations, where the risk of sheering off the hydrophilic coating is theoretically higher 2,5. This may also explain why the use of flow-diverting stents, although the devices are nowadays very flexible and soft, are over-represented in reported cases as flow diverters have to be pushed out of a tight fitting sheath and microcatheter 2.
Of note, it has been theorized that the same mechanism may be responsible for delayed intraparenchymal hemorrhage (DIPH) following aneurysm repair 3 although other theories also exist.
Radiographic features
NICE lesions are typically only seen in the territory corresponding to the vessel that was the target of endovascular therapy 1. Variations in circle of Willis anatomy can therefore influence the distribution of lesions.
CT
Non-contrast CT may be normal or demonstrate small areas of hypodensity 1.
MRI
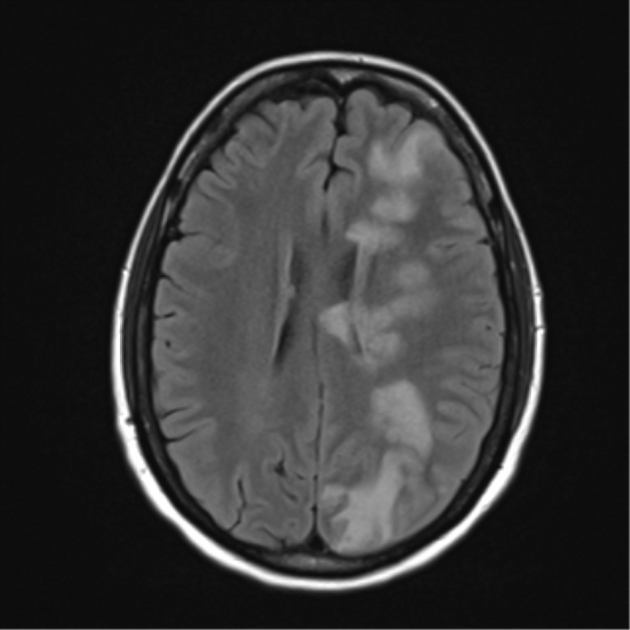
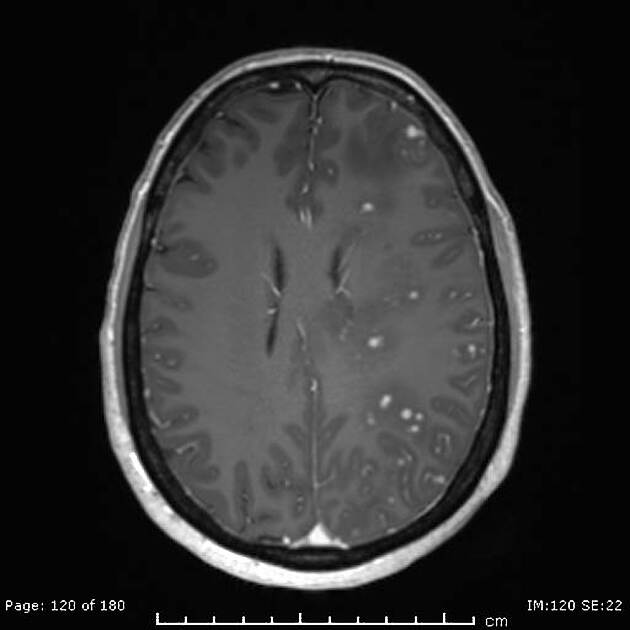
NICE lesions appear as multiple punctate or small ring enhancing foci. They can involve the white matter, cortex or leptomeninges 1. They have the following signal characteristics 1:
T1: hypointense
-
T2
central iso- to hypointense
peripheral hyperintensity due to vasogenic edema
DWI/ADC: variable
SWI/T2*: variable, some normal other show signal loss
Angiography (DSA)
No angiographic features have been described 1,2.
Treatment and prognosis
The natural history of NICE lesions remains to be established. Corticosteroids can reduce edema and enhancement, however, recurrence may occur and thus follow-up with MRI is recommended 1. Antiseizure medications may be necessary in patients with seizures 5.
Differential diagnosis
subacute infarcts: may appear similar, however, would be expected to appear immediately following the procedure and will undergo expected evolution
cerebral microabscesses: may appear similar on imaging but are usually encountered in a different clinical scenario and would not be expected to be confined to the vascular territory of prior treatment




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.